SPA Board of Directors Candidates
Click here to cast your vote (SPA member username/password required)
President
 Full Name:
Full Name:
Nancy L. Glass, MD, MBA, FAAP
Name and City/State of Hospital/Institution for which you work.
Texas Children’s Hospital and Baylor College of Medicine, Houston, TX
Hospital/Institution Titles:
Professor of Anesthesiology and Pediatrics, Baylor College of Medicine; Director, Anesthesia Education and Pediatric Anesthesia Fellowship, Director, Pediatric Pain Service, Texas Children's Hospital.
Name and City/State of College attended; degree and year obtained:
Rice University, Houston, TX, BA 1986 (real year, long story there!)
Name and City/State of Medical School attended, degree and year obtained:
Baylor College of Medicine, Houston, TX, MD, 1978.
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained:
Baylor College of Medicine Affiliated Hospitals, Pediatrics, 1978 – 1981.
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training:
University of Texas Health Science Center at Houston, Houston, TX, 1986-1987.
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship:
Children’s National Medical Center, Washington, DC, Pediatric Critical Care Medicine, 1981-1983.
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training:
Rice University, Houston, TX, MBA, 2002.
Prior involvement with SPA (Board, Committee, etc) (if applicable) please provide a brief description of these activities:
Presenter of PBLDs, abstracts, and Workshops (Epidural and Peripheral Blocks); Board Member, 2000-2004; Winter Meeting Program Chair, 2005 and 2006. Secretary, 2006-2008, Treasurer, 2008-2010, Vice President, 2010-2012. Member, Education and Finance and Membership Committees; Member, Executive Committee.
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) please provide a brief description of organization:
Member, ASA; Member, ASRA, Member, ASA Sub-Committee on Pediatric Program.
Vice President
 Full Name
Full Name
Shobha Malviya, MD, FAAP
Name and City/State of Hospital/Institution for which you work.
University of Michigan Health System, Ann Arbor, MI
Hospital/Institution Titles.
Professor of Anesthesiology, Associate Director of Pediatric Anesthesiology, Director of Pediatric Anesthesia Research
Name and City/State of College attended; degree and year obtained.
Jai Hind College and Basantsingh Institute of Science, Bombay University
Mumbai/Maharashtra/India
Inter Science Degree 1975
Name and City/State of Medical School attended, degree and year obtained.
Topiwala National Medical College, Bombay University
Mumbai/Maharashtra/India
MBBS, 1981
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
St. Luke’s Roosevelt Medical Center, NY, NY
Pediatrics Internship, 07/01/1981 – 06/30/1982
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
University of Michigan Health System, Ann Arbor, Mi
07/01/1985 – 06/30/1987
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
Hospital for Sick Children, Toronto, Ontario, Canada
08/01/1987 – 07/30/1988
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
Rainbow Babies’ and Children’s Hospital, Cleveland, OH
Pediatrics Residency, 07/01/1982 – 06/30/1984
Prior involvement with SPA (Board, Committee, etc) (if applicable) please provide a brief description of these activities.
Committee memberships and chair positions:
1994-present - SPA member
1998-2004 - Member, Subcommittee on Publications
2004-2008 - Member, Board of Directors
2005-2008 - Co-Chair, Communications Committee
2008-2010 - Secretary
2008-present - Chair, Membership Committee
2010-present - Secretary/Treasurer
2010-present - Chair, Finance Committee
2008-present - Member, Executive Committee
2008-present - Member, Finance Committee
2009-present - Member, Education Committee
2009-present - Member, Enduring Materials Committee
Educational activities:
2003 - Refresher Course lecture
2004 - Delivered lecture at AAP breakfast panel
2005 - Faculty, Success in Academics Workshop
2006 - Lecture at annual meeting
2009 - Lecture at Fundamentals course
2011 - Lecture at Fundamentals course
2011 - PBLD
Other SPA related activities:
- Presented numerous research abstracts
- Contributions to newsletter and website
- Redesigned website during tenure as communications committee chair
- Moderated several poster sessions
- Attended SPA strategic planning meeting in Chicago IL
- 100% attendance at board meetings and executive committee meetings
- Participation in all teleconferences for board of directors and executive committee
- Reviewer of submitted abstracts on a regular basis
- Reviewer of PBLD
Secretary/Treasurer:
 Full Name:
Full Name:
Randall Paul Flick, MD, MPH, FAAP
Name and City/State of Hospital/Institution for which you work.
Mayo Clinic, Rochester, MN
Hospital/Institution Titles.
Mayo Clinic Children’s Center
Chair, Division of Pediatric Anesthesiology
Medical Director, Eugenio Litta Children’s Hospital
Chief Quality Officer Mayo Clinic Children’s Center
Vice-Chair for Quality Department of Pediatrics and Adolescent Medicine
Name and City/State of College attended; degree and year obtained.
St. Luke’s Hospital’s School of Nursing, Fargo, ND - R.N., 1980
Moorhead State University, Moorhead, MN - B.A., 1983
Johns Hopkins University, Baltimore, MD - M.P.H., 1995
Name and City/State of Medical School attended, degree and year obtained.
University of North Dakota, Grand Forks, ND - M.D., 1987 (AOA)
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
St. Louis Children’s Hospital, St. Louis, MO - Pediatrics, 1987-90
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
Barnes Hospital-Washington University, St. Louis, MO, 1990-92
Johns Hopkins University, Baltimore, MD, 1992-93
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
Johns Hopkins University - Pediatric Anesthesiology, 1992-95
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
Johns Hopkins University - Pediatric Critical Care, 1992-95
(Fellowships in CCM and pediatric anesthesia were concurrent)
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
Member - 1996 - present
Committee involvement:
Education Committee
SPACIES
By-Laws (Chair)
Program Chair
Winter - 2007
Winter - 2008
Fundamentals - 2009
Fundamentals - 2010
International Assembly - 2012
Board of Directors - 2008 – present
My involvement with the SPA has been extensive including consistent involvement in the education committee leading to appointment as program chair for the 2007 - 2008 winter meetings. Subsequently, I promoted the development and chaired the Fundamentals meetings that will resume as a comprehensive review this year. I have been involved in the conception and development of the International Assembly to be held in Washington this year. The meeting is certain to be the largest international meeting of pediatric anesthesiologists ever held. Chairing the IAPA program has required coordination with the ASA, WFSA as well as multiple pediatric societies and key leaders from around the world. It also includes a special article in Anesthesia and Analgesia, a special edition of Pediatric Anesthesia and a Scholars Program that has raised funds to assist young pediatric anesthesiologists from around the world.
The IAPA and my involvement at the SPA have been a labor of love. The meeting represents my view that the SPA has the opportunity to move into a position of international leadership. Increasingly, the membership and leadership of all of the various societies of the world must begin to work together to promote education, research and most importantly high quality, safe and effective care for children regardless of where in the world they live.
In addition to my involvement in creating and conducting educational content, I have contributed to the enduring materials and with SPACIES created a set of guidelines for the provision of care on short term medical missions in the less developed world. These guidelines have been adopted by the SPA, as well as the plastic surgical, cleft lip and palate and maxillofacial societies and have been published in the respective journals of the societies.
As a member of the board and Chair of the By-Laws Committee I have rewritten and/or revised significant portions of the current by-laws and assisted in revising the structure of the Winter Meeting finances with the goal of making the meeting self-sufficient.
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization.
ASA -
Vice Chair Scientific Content Subcommittee for Pediatric Anesthesia – This is the committee that creates all of the pediatric content for the ASA Annual meeting. I will assume the position of Chair this fall.
IARS -
I was asked by the SPA board to represent them at the SmartTots advisory board. SmartTots is a public private partnership between the US FDA and the IARS devoted to funding a promoting research related to anesthetic related neurotoxicity in children.
US FDA -
Current Chair of the Anesthetic, Analgesic Drug Product Advisory Committee (AADPAC) for the US Food and Drug Administration. This is the committee at the FDA that reviews for approval all drugs for use as analgesics and anesthetics in the US. It oversees the FDA response to concerns regarding use and misuse of narcotics, drug shortages, and the potential neurotoxicity of anesthetic agents.
AAP-
Member of the AAP Committee on Anesthesia and Pain Management and will represent the AAP and SPA as a plenary speaker at this years AAP meeting.
MSA-
As a member of the Minnesota society of Anesthesiologists I led a group that created a set of guidelines for the care of children in Minnesota operating rooms. Minnesota is one of only two states with such guidelines.
ASPS -
For several years I served as the only non-plastic surgeon on the VIPS (Volunteers in Plastic Surgery) steering committee. This is the committee that oversees all volunteer activity for the Society and reviews grants for Smile Train. My contribution to the group was to provide insight into patient safety and co-author guidelines for safe care that have been broadly adopted by ASPS and several other organizations including the SPA.
SNI -
Smile Network International is an organization devoted to the care of children in the less developed world. As a member of the Board and the Medical Director I wrote the majority of the existing care protocols, organized mission staffing, interacted with donors, and assisted in overall oversight of the organizations activities.
PAPD -
The Pediatric Anesthesia Program Directors committee is now a part of the SPA. Previously this group was independent and oversaw the activities of pediatric anesthesia fellowship programs. My role was as president – elect. I stepped down from that role in order to allow my assistant PD to assume the role of PD at Mayo.
AASPD -
As a former program director and president elect of the PAPD I served as a member of the AASPD (Association of Anesthesiology Subspecialty Program Directors).
ABA -
The American board of Anesthesiologists recently convened a group to write the upcoming pediatric anesthesia subspecialty board examination. As a member of that group I have participated in the writing and editing of questions for that exam.
 Full Name
Full Name
Julie Jan Niezgoda, MD
Name and City/State of Hospital/Institution for which you work.
Cleveland Clinic
Cleveland, Ohio
Hospital/Institution Titles.
Staff Department of Pediatric Anesthesia
Staff Department of Pediatrics
Assistant Program Director Pediatric Anesthesia Fellowship
Name and City/State of College attended; degree and year obtained.
The Ohio State University
Columbus, Ohio
Bachelor of Science 1979
Name and City/State of Medical School attended, degree and year obtained.
The Ohio State University
Columbus, Ohio
Doctor of Medicine 1985
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
Department of Anesthesiology Case Western Reserve University
Cleveland, Ohio 1988
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
Department of Anesthesiology Case Western Reserve University
Cleveland, Ohio 1988-1991
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
University of Pittsburgh
Children’s Hospital of Pittsburgh,
Pittsburgh, PA
Pediatric Anesthesia Fellowship 1992-1993
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
Rainbow Babies and Children’s Hospital
Case Western Reserve University
Cleveland Ohio
Pediatric Residency 1985-1988
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
Board of Directors SPA- 2008-present
Assistant Program Chair (PBLD coordinator) 2009 Jacksonville Winter meeting
Assistant Program Chair (PBLD coordinator) 2010 San Antonio Winter Meeting
Assistant Program Chair (Refresher/Workshop coordinator) 2011 San Diego Winter Meeting
Program Chair 2012 Tampa Winter Meeting
Member Education Committee 1999-present
SPA invited speaker/workshop participant/moderator 2008, 2011, 2012
Speaker SPA Fundamentals of Pediatrics Course 2011
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization.
Healing the Children Participated in 8 International Missions-Guatemala & Honduras 2003-2010
Esperanza 1 mission Bolivia 2011
Directors-At-Large – Three open positions
 Full Name.
Full Name.
Franklyn P. Cladis, MD
Name and City/State of Hospital/Institution for which you work.
The Children’s Hospital of Pittsburgh of UPMC, Pittsburgh PA,
The University of Pittsburgh Medical Center
Hospital/Institution Titles.
Assistant Professor of Pediatrics
Program Director, Pediatric Anesthesiology Fellowship
Name and City/State of College attended; degree and year obtained.
University of Pennsylvania, BA, 1991
Name and City/State of Medical School attended, degree and year obtained.
University of Rochester, MD, 1995
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
University of Rochester, Internal Medicine internship and residency, 1995-1998
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
University of Rochester, Anesthesiology Residency, 1998-2001
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
The Children’s Hospital of Boston, Pediatric Anesthesiology, 2001-2002
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
- Education Committee member -2006 to present. My involvement with the education committee has included attending education committee meetings, grading PBLD’s and moderating poster sessions. My goal is to gain experience to eventually become a program director for a meeting.
- Enduring material sub-committee member-2008-2010. This committee was involved with creating enduring material from the society’s meetings. The material was organized into multiple choice questions with detailed answers.
- Pediatric advanced life support instructor (winter meetings)- 2006-present
- Pediatric Anesthesia Program Directors Association (PAPDA)-I served as the secretary for this organization from 2010 to 2011. In 2011, I was elected to the PAPDA board as one of the Members-at-Large, where I continue to serve in this capacity.
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization.
- American Board of Anesthesiology-Pediatric examination writing committee 2012. I participated in the exam writing process for the ABA Pediatric Anesthesiology Board Exam.
- Smith’s Anesthesia for Infants and Children 8th edition-Co-editor, 2011
- openanesthesia.org - Section Editor, Pediatric Anesthesia
 Full Name
Full Name
Randall M. Clark, MD
Name and City/State of Hospital/Institution for which you work.
University of Colorado School of Medicine, Anschutz Medical Campus, Aurora, CO
Hospital/Institution Titles.
Associate Professor and Chief, Section of Pediatric Anesthesiology,
Department of Anesthesiology, University of Colorado School of Medicine
Chair, Department of Anesthesiology,
Children’s Hospital Colorado
Name and City/State of College attended; degree and year obtained.
University of Colorado, Boulder, Colorado
Bachelor of Science with Honors, Aerospace Engineering Sciences, 1978
Name and City/State of Medical School attended, degree and year obtained.
University of Colorado School of Medicine, Denver, Colorado
Doctor of Medicine, 1982
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
Baylor College of Medicine, Houston, TX
General Surgery, 1982-1985
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
Baylor College of Medicine, Houston, TX
Anesthesiology, 1985-1987
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
Baylor College of Medicine, Houston, TX
Cardiovascular Anesthesiology, Jul-Dec 1987
Pediatric Anesthesiology, Jan-Jun 1988
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
N/A
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
I have had the great pleasure of previously serving the members of SPA as an ex officio member of the Board of Directors during my term as the Chair of the ASA Committee on Pediatric Anesthesia. My primary aim during my tenure was to improve the communication and coordination between the three great bodies representing anesthesiology and pediatric anesthesiologists in this country; ASA, SPA, and the AAP Section on Anesthesiology and Pain Medicine. I believe we were quite successful in many of the activities from that time which included close coordination around the FDA hearings on the effects of anesthetic agents on the developing brain, advocacy for education and oversight in the realm of deep sedation by non-anesthesiologists, and the many discussions about subspecialty certification in pediatric anesthesia. I am very enthusiastic about the possibility of returning to the SPA Board as a full member.
I have also had the opportunity to serve on the SPA Committee on Governmental Affairs. My primary effort there and in parallel committees with ASA and my state society has been to advocate for proper positioning of pediatric anesthesiology in the Medicaid payment structure. The future health of our specialty and our ability to serve our patients depends on a sound financial footing. Health care reform with its dramatic expansions of the Medicaid program and its innovations such as Accountable Care Organizations serves as both a great potential threat to our specialty and a great opportunity to address these challenges. Organizations like SPA and its Board of Directors will be instrumental in meeting these challenges. I hope to be part of it.
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization.
In concert with many of the chairs of the departments of anesthesiology in the nation’s freestanding children’s hospitals and the chiefs of the sections of pediatric anesthesiology in many of the nation’s academic anesthesiology programs, I helped found and organize what is now called the Pediatric Anesthesiology Leadership Council (PALC). This group, which receives great support from SPA, now meets twice a year. The chiefs and chairs sit at the confluence of many important aspects of our specialty. They may have responsibility for clinical services in many of our hospitals, oversight of our residency and fellowship programs, and the fostering of research. Through information sharing, common problem solving, and advocacy, PALC attempts to strengthen our departments of anesthesiology, and through them, to advance our specialty.
 Full Name
Full Name
Ira Todd Cohen, MD, MEd, FAAP
Name and City/State of Hospital/Institution for which you work
Children's National Medical Center
George Washington University
Washington, DC
Hospital/Institution Titles.
Director of Education
Program Director Pediatric Anesthesiology Fellowship
Professor of Anesthesiology and Pediatrics
Name and City/State of College attended; degree and year obtained.
Connecticut College
New London, CT
BA: 1975-1979
Name and City/State of Medical School attended, degree and year obtained.
New York University
School of Medicine
New York, NY
MD: 1979-1983
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
Einstein Affiliated Hospitals (Pediatrics)
Albert Einstein College of Medicine
Bronx, NY
Pediatrics: 1983-1984
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
New York University
School of Medicine
New York, NY
1985-1988
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
Children's National Medical Center
George Washington University
Washington, DC
Pediatric Anesthesiology: 1989
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
Einstein Affiliated Hospitals
Bronx, NY
Pediatrics: 1983-1986
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
SPA Board of Director: 2009-present
Education Committee
Enduring Materials Subcommittee
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization.
Society for Education in Anesthesia: President-Elect
(The SEA is an organization for anesthesiologists who strive to enhance their abilities and scholarly endeavors in the field of education.)
Pediatric Anesthesia (Fellowship) Program Directors Association
 Full Name
Full Name
Joseph P. Cravero, MD, FAAP
Name and City/State of Hospital/Institution for which you work.
Geisel School of Medicine
Dartmouth Hitchcock Medical Center
Lebanon, NH 03756
Hospital/Institution Titles.
Professor of Anesthesia and Pediatrics
Director of Pediatric Anesthesia
Director of the Pediatric PainFree Program
Vice Chair Department of Anesthesiology
Name and City/State of College attended; degree and year obtained.
Holy Cross College
Worcester MA
BA Chemistry, 1982
Name and City/State of Medical School attended, degree and year obtained.
University of Virginia, MD, 1986
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
Fitzsimmons Army Medical Center – 1986-87
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training
Hartford Hospital 1993-1996
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
Residency in Pediatrics – Fitzsimons Army Medical Center, Aurora, CO 1987-89
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
Currently serving as Liaison to the American Academy of Pediatric Dentistry Sedation Taskforce for the SPA Board.
I have been involved with the Quality Assurance Committee for several years – particularly involving sedation issues.
Over the last 16 years I have served been involved with the education committee and the various iterations of the research committee.
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization.
I served on the executive board of the American Academy of Pediatrics Section on Anesthesiology and Pain Medicine for 14 years – starting as a liaison for the Committee on Pediatric Emergency Medicine – subsequently as a board member, and finally as Chair of the Section. In this capacity I was very involved with planning of the SPA/AAP Winter Meeting and the educational offerings of the AAP SOA at the SPA meetings as well as at the AAP and ASA annual meetings. My primary goal in these efforts has been to seek improvement in children’s health care through a collaborative and inclusive approach.
I founded the Pediatric Sedation Research Consortium (PSRC) and subsequently the Society for Pediatric Sedation (SPS) in an attempt to help improve the delivery of sedation care to children in all clinical venues. The PSRC has subsequently become a resource for outcomes based research in this area of clinical care and the SPS is a thriving organization with 700 members (physicians and nurses) from a variety of specialties that deliver sedation care. The mission of both organizations is to use data sharing and collaboration to identify problem areas and solutions for children undergoing sedation for procedures and tests.
 Full Name
Full Name
Kirk Lalwani, MD, FRCA, MCR
Name and City/State of Hospital/Institution for which you work.
Oregon Health and Science University,
Portland, Oregon
Hospital/Institution Titles.
Associate Professor, Anesthesiology and Pediatrics,
Director, Pediatric Anesthesiology Fellowship Program.
Attending Physician, Doernbecher Children's Hospital / Oregon Health and Science University.
Chair, Resident Evaluation and Clinical Competence Committee,
Department of Anesthesiology and Perioperative Medicine.
Oregon Health and Science University.
Name and City/State of College attended; degree and year obtained.
1979-1981 - Pre-University Certification, The National College, Bangalore, India
Name and City/State of Medical School attended, degree and year obtained.
1981-1986 - St. John’s National Academy of Medical Sciences, Bangalore, India
Bachelor of Medicine and Bachelor of Surgery (MBBS), 1988.
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
8/86-8/87 - Transitional rotating internship (12 months)
St. John's Medical College Hospital, Bangalore, India
Bachelor of Medicine and Bachelor of Surgery (MBBS), 1988.
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
1990-1991 - Senior House Officer in Anesthesia, Norfolk and Norwich Hospital, UK
- Registrar in Anesthesia, Norfolk and Norwich Hospital, UK
- Registrar in Anesthesia, Greenwich District Hospital, London, UK
- Registrar in Anesthesia, The Brook General Hospital, London, UK
- Acting Senior Registrar, The Brook General Hospital, London, UK
3/95- 4/9 - Registrar in Anesthesia, King’s College Hospital, London, UK
5/95-7/95 - Senior Registrar in Anesthesia, St. Andrew’s Hospital for Burns and Plastic Surgery, Essex, UK
8/95-10/95 - Senior Registrar in Anesthesia, The Royal London Hospital.
Lecturer, Academic Department of Anesthesia, Royal London Hospital
4/97-5/97 - Senior Registrar, The London Chest Hospital, Bonner Rd., London
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
11/95-10/96 - Senior Registrar / Fellow in Pediatric Anesthesia,
Great Ormond Street Hospital for Children, London, UK
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
9/87- 5/88 - Demonstrator in Anatomy,
St. John’s National Academy of Medical Sciences, Bangalore, India
6/88-11/88 - Senior House Officer, Coronary Care Unit/Cardiology,
St. John’s National Academy of Medical Sciences, Bangalore, India
11/88-5/89 - Senior House Officer, Intensive Care Unit/Internal Medicine,
St. John’s National Academy of Medical Sciences, Bangalore, India
1992 - Advanced Trauma Life Support Provider Course, Tunbridge Wells, UK
Fellow of the Royal College of Anesthetists (FRCA), UK
Certificate of Completion of Specialist Training in Anesthesia, UK
2002-2004 - Certificate in Human Investigations Program, Oregon Health and Science
University, Portland, Oregon, USA
2005- 2008 - Master of Clinical Research (M.C.R.), Oregon Health and Science University.
2008-Present - American Board of Anesthesiology Alternate Pathway Certification:
Candidate in the ABA Examination system (previously termed Board Eligible)
2009 - Advanced Cardiac Life Support Provider Course, OHSU
2011 - Pediatric Advanced Life Support Provider Course, OHSU
2012 - Certificate in Medical Education Research (MERC),
Association of American Medical Colleges.
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
Society for Pediatric Anesthesia/American Academy of Pediatrics Joint Winter Scientific Meetings: Faculty, Difficult Airway Workshop: 2005, 2007, 2008.
Workshop Co-Director (with Dr. Nancy Glass): How to Write and Moderate a Great PBLD: 2012, 2013.
Pediatric Anesthesia Program Directors' Association- since inception
Participated in committee activities, was part of a taskforce exploring Advanced Pediatric Fellowship Program development.
Society for Pediatric Anesthesia: Education Committee, 2010-current
Reviewer for PBLD submissions for the Scientific Meetings (2010-2012)
Reviewer for scientific abstract submissions for the Scientific Meetings (2010-2011)
SPA/AAP Joint Winter Scientific Meeting: Planning Committee, 2010-2013
a. PBLD Coordinator, SPA/AAP Joint Winter Scientific Meeting: Planning Committee, 2010-11
b. Workshop Coordinator and Program Co-Chair, SPA/AAP Joint Winter Scientific Meeting: Planning Committee, 2011-12
c. Program Chair, SPA/AAP Joint Winter Scientific Meeting: Planning Committee, 2012-13
I was elected to a 3-year term on the planning committee, commencing 2010. With the assistance of the Program Chair, Co-Chair, SPA President, and the SPA administrative staff, I was responsible for coordinating the submission, review, and selection of PBLDs for the annual meeting in my first year. I made changes to the submission criteria that added clarity to the content and quality of the submissions.
The second year I was responsible for coordinating the selection of the workshops. This year, I am currently in the process of finalizing the selection of speakers and the 2013 meeting program. My responsibilities include liaising with the AAP President and AAP Education Committee Chair for the AAP sections of the program, overseeing the efforts of the PBLD Coordinator and Program Co-Chair in arranging the PBLDs and Workshops, ensuring that the program meets the needs of our members, and that it is ready on time. Once again, the excellent administrative assistance from the staff at SPA and the guidance of the SPA President have been invaluable in this process.
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization.
American Society of Anesthesiologists: PBLD Committee, 2010-current
The Royal College of Anaesthetists, London, U.K.: Fellow
Society for Education in Anesthesia
 Full Name
Full Name
Mary Ellen McCann, MD, MPH
Name and City/State of Hospital/Institution for which you work.
Boston Children’s Hospital
Boston, Massachusetts
Hospital/Institution Titles.
Senior Associate in Anesthesiology,
Department of Anesthesia, Perioperative and Pain Medicine
Boston Children’s Hospital
Associate Professor of Anaesthesia
Harvard Medical School
Name and City/State of College attended; degree and year obtained.
Boston University
Boston, MA
Boston University Six Year Program in Medicine
1981-BA and MD
Name and City/State of Medical School attended, degree and year obtained.
Boston University
Boston, MA
Boston University Six Year Program in Medicine
1981-BA and MD
Name and City/State of Hospital where Internship was completed; type and dates attended; degree and year obtained.
Massachusetts General Hospital
Boston, MA
Internship and Residency in Pediatrics
1981-1984
Name and City/State of Hospital where Anesthesiology Residency was completed; dates of training.
Massachusetts General Hospital
Boston, MA
Residency in Anesthesia
1986-1988
Name and City/State of Hospital where Fellowship training was completed (if applicable); type and dates of Fellowship.
Massachusetts General Hospital
Boston, MA
Clinical Research Fellowship in Pediatric Anesthesia
1988
Name and City/State of Hospital/University where additional training was completed (if applicable); type and dates of training.
Harvard University School of Public Health
Boston, MA
2004-2005 MPH
Prior involvement with SPA (Board, Committee, etc) (if applicable) – please provide a brief description of these activities.
I have been a member of the SPA since 1998 and a member of the education committee since 2003. I was Vice Chair of the 2009 and 2010 Winter Meetings and Chair of the 2011 Winter Meeting in San Diego.
My other contributions include submissions for the Enduring WEB based learning (Reflex Sympathetic Dystrophy and Is nitrous oxide a safe anesthetic?) as well as Lecture Series Power Point Presentations
The SPA has been invaluable to me as a clinical investigator. The contacts and interactions that I made through the SPA were instrumental in creating the US consortium (10 pediatric academic centers in the US) for the GAS trial (a pediatric RCT anesthetic neurotoxicity trial). In addition, the support of the SPA leadership was helpful in obtaining funding from the FDA and NIH for this trial. The Education Committee and biannual SPA meetings have fostered several collaborations with other like-minded members who are interested in outcomes research.
Involvement with other national/international (pediatric) anesthesia organizations (if applicable) – please provide a brief description of organization
I have worked with the ASA subcommittees and committees on Pediatric Anesthesia and Infection Control. I have been the pediatric representative to the ASA Task Force on Infection Control since 2003. Last year we published the 3rd Edition ASA RECOMMENDATIONS FOR INFECTION CONTROL FOR THE PRACTICE OF ANESTHESIOLOGY. I also was a member of the Surgical Infection Prevention Collaborative sponsored by the Children’s Hospital and Child Health Corporation of America from 2006-2007. My work on these committees stem from my interest in infection control during anesthesia and critical care.
My ASA involvement also includes membership on the Subcommittee for Pediatrics from 2003-2005 and Pediatric Anesthesia Committee in 2008-2009. Last year I became a member on the Education Track Subcommittee on Pediatric Anesthesia and a member of the ASA Abstract Review Subcommittee on Pediatric Anesthesia.
I also am involved in the FDA’s Task Force on Epidemiologic Studies of Anesthetic Neurotoxicity since 2007. This group meets periodically to review ongoing research and evidence on this topic.
I served as a faculty member at several international pediatric congresses in the Netherlands, Italy and the United Kingdom. My lectures included topics such as anesthetic-induced neurotoxicity, neonatal encephalopathy and anesthesia for the newborn.
I have been a longtime member of the Joint Commission of Women in Medicine at Harvard Medical School. My areas of expertise are improving the status of part-timers in academic medicine and mid career entry into academic medicine.
Summer Renewal
Summer time is time for family vacations, new trainees and very busy operating room schedules. It is also the season of the year when living in Seattle is pure joy. I hope others are weathering the heat and/or rain that this season brings to your homes.
Summer is also the time to renew and revise the SPA leadership team. As you will note in this edition of the SPA Newsletter, the slate of candidates for the election of the next Secretary-Treasurer and three at-large positions on the Board of Directors has been established. The nominations committee has presented the membership with a list of very qualified and capable candidates that have demonstrated their commitment to our specialty of pediatric anesthesia and society.
Candidates for the position of Secretary-Treasurer are Randall Flick (Mayo Clinic) and Julie Niezgoda (Cleveland Clinic). The list of candidates for the three positions on the Board opening for election include: Franklyn Cladis - Children’s Hospital of Pittsburgh; Randall Clark – Denver Children’s Hospital; Ira Todd Cohen – Children’s National Medical Center (Washington DC); Joseph Cravero – Dartmouth-Hitchcock Medical Center; Kirk Lalwani – Oregon Health Sciences University; and Mary Ellen McCann – Children’s Hospital Boston.
This is an amazing group of dedicated and accomplished physicians with diverse interests and backgrounds all committed to improving perioperative care for children. The electronic election process is open and will remain open until September. I would encourage all members of SPA to take the time to carefully review the bios of each candidate in this newsletter or on the SPA website (http://www.pedsanesthesia.org/) and then vote for the next generation of leaders that will move the society forward.
Let me also express my thanks and gratitude to the members of the Nominations Committee (Chair – Joe Tobin, Allison Kinder-Ross, Frank McGowan, Shobha Malviya, and Santhanam Suresh) for all of their time and effort finding us this great group of leaders in our specialty.
A focus of concentrated effort and hard work over many years by a large number SPA members and leaders has been our ultimately successful campaign to get approval of an American Board of Anesthesiology (ABA) certification process for Pediatric Anesthesia. Frank McGowan and Joe Tobin were two of the key players in this multiyear collaborative effort. The fruits of these labors are now in place. In this edition of the SPA newsletter is an update from Mark Rockoff, ABA President outing the new certification process. The first pediatric certification examination will be administered on October 19, 2013. For additional information and to begin the application process, go to the ABA website (http://www.theaba.org/home/examinations_certifications).
The Society for Pediatric Anesthesia is hosting the International Assembly for Pediatric Anesthesia (IAPA) Meeting in honor of our 25 years of support to children in the perioperative setting. The theme for the IAPA meeting is “Safety Knows No Borders” and the meeting format will expand from one to two days (Thursday and Friday October 11-12, 2012) to include featured lectures, workshops, digital poster sessions, panel and problem based learning discussions with participants from every continent around the world (http://www.internationalassembly2012.org/program.html).
This conference also includes a program to facilitate attendance by international pediatric anesthesia providers called the International Scholars Program. Successful applicants will receive fiscal support ($2,500) to offset a portion of their travel-related expenses for this trip, free complimentary registration at the IAPA and American Society of Anesthesiologists (ASA) meetings, and an invitation to the IAPA Faculty VIP Dinner on Thursday October 11th.
Sponsoring organizations from around the world have contributed funds to support 34 scholars from 23 countries (Bangladesh, Bhutan, China, Columbia, Ethiopia, Fiji, India, Kenya, Mexico, Mozambique, Nepal, Nigeria, Pakistan, Papua New Guinea, Peru, Samoa, Serbia, Solomon Islands, South Africa, Tunisia, Uganda, Ukraine and West Africa). My personal thanks to the 24 sponsoring organizations listed below:
Sponsors/Hosts
Ann & Robert H. Lurie Children’s Hospital of Chicago
Arkansas Children’s Hospital
Children’s Healthcare of Atlanta (Egleston/Emory)
Children’s Hospital Boston
Children’s Hospital Colorado
Children’s Hospital of Los Angeles
Children’s Medical Center Dallas
Children’s National Medical Center
Cincinnati Children’s Hospital
Cleveland Clinic
Geneva Children’s Hospital
Johns Hopkins Hospital
Massachusetts General Hospital
Mayo Clinic
Operation Smile
Seattle Children’s Hospital
Society of Pediatric Anesthesia of New Zealand and Australia
Stanford University
Texas Children’s Hospital
University of California, Irvine
University of Michigan CS Mott Children’s Hospital
University of Virginia Medical Center
Valley Anesthesiology Consultants (Phoenix)
Commercial Supporters
Nonin
PAJUNK
The meeting will be held in the Marriott Wardman Park Hotel in Washington D.C. I strongly encourage all SPA members to take advantage of our low group rates at the meeting hotel in a very pleasant part of the city with many fine restaurants, the national zoo and direct access to the Metro (subway). All IAPA attendees staying at the Marriott Wardman Park will receive a free Metro Card to facilitate transportation throughout the Washington D.C. area during your stay.
As part of the 25th anniversary celebration of the Society for Pediatric Anesthesia, the SPA Board of Directors is asking all of our members to consider making a pledge of support for the Patient Safety, Education & Research Fund. The SPA Board of Directors has decided to match all donations for the entire calendar year of 2012 dollar for dollar.
Thus, a $500 personal donation will result in a $1,000 contribution to the Patient Safety, Education & Research Fund. We have pledges from 100% of current officers and board members, past presidents, and our former board members. Please take advantage of this time limited opportunity to further the capabilities for SPA to have a positive impact on the perioperative care of children around the world.
All charitable contributions to this fund are tax deductable. Please consider this fund as you create your charitable giving plan for the year. You can make your electronic donation at http://www.pedsanesthesia.org/researchfunddonate.iphtml. Contact Kim Battle, SPA Association Manager, at kim@societyhq.com or fax to 804-282-0090 if you have questions.
I hope to see you all this fall in Washington, DC as we culminate the celebration of our first 25 years of service to children!
A Window on SPA
It’s summer, which probably means busier-than-ever operating rooms wherever this newsletter finds you. As with every edition, this one’s a window through which we see the many activities of our society and our sub-specialty.
From a society perspective, you will find excellent reviews of our 2012 winter meeting, held in Tampa, Florida. I’m indebted to the communication committee members who provide these reviews every year. Also, it’s board election time, so nominee’s biographies are available for your review. To quote Al Capone, “Vote early and vote often”… well, maybe just vote early.
The International Assembly for Pediatric Anesthesia (Safety Knows no Borders) will soon be upon us. If you haven’t done so already, be sure to make arrangements to join your colleagues and friends in Washington, DC from October 11-12.
Subspecialty certification in pediatric anesthesia is a hot topic. Be sure to read the update from Mark Rockoff MD, Associate Anesthesiologist-in-Chief at Boston Children’s Hospital and President of the American Board of Anesthesiology.
Later in the newsletter, we mourn the loss of a colleague, Dr. Mark Rossberg, but also celebrate examples of the bright talent attracted to our profession: Ms. Connolly (youngest SPA presenter) and Dr. Buscetta (a beautiful piece of creative writing that reminds me why I love being a pediatric anesthesiologist).
Returning to the topic of busy work schedules, I do hope that you find time this summer to enjoy some fine weather, great company and the pleasure of a favorite pursuit or hobby. If not before, I look forward to seeing you all in Washington, DC in the fall.
Certification in Pediatric Anesthesiology
The American Board of Anesthesiology (ABA) has been authorized by the American Board of Medical Specialties (ABMS) to offer certification in the subspecialty of Pediatric Anesthesiology. The ABA already offers certification in the subspecialties of Critical Care Medicine, Pain Medicine, Hospice and Palliative Medicine, and Sleep Medicine. Applications will be accepted through February 15, 2013 for the first pediatric anesthesiology certification examination which will be administered on October 19, 2013 (and annually thereafter).
Physicians who apply for subspecialty certification in pediatric anesthesiology must:
- Hold an unexpired license to practice medicine or osteopathy in at least one state or jurisdiction of the United States or Canada that is permanent, unconditional and unrestricted;
- Be a diplomate of the ABA;
- Be a participant in the ABA's Maintenance of Certification in Anesthesiology Program (MOCA®);
- Have satisfactorily completed fellowship training in pediatric anesthesiology or possess the required experience in pediatric anesthesiology as described below.
Fellowship Training
Satisfactory completion of a one-year fellowship program in pediatric anesthesiology that was ACGME-accredited throughout the time of enrollment, with verification from the program director.
OR
"Grandfathering" Criteria
(Only for diplomates who completed anesthesiology residency training before July 1, 2012)
An anesthesiologist’s clinical practice has been devoted primarily to pediatric anesthesiology for the last 2 years, or at least 30% of an anesthesiologist’s clinical practice, averaged over the last 5 years, has been devoted to pediatric anesthesiology. The anesthesiologist’s practice must include neonates and children under the age of 2 years and procedures considered high-risk. Attestations from the applicant as well as the applicant’s Department Chair (or other institutional official if the applicant is the Department Chair) that the applicant meets these practice requirements will be required.
Note: The ABA’s Credentials Committee may request further documentation of an applicant’s clinical practice, including case logs. Furthermore, "grandfathering" criteria will be applicable only through the certification examination in pediatric anesthesiology in 2015, after which authorized fellowship training in pediatric anesthesiology will be required. All candidates, including those who qualify via "grandfathering" criteria, must take and pass the subspecialty examination.
The pediatric anesthesiology examination will consist of multiple-choice questions designed to broadly assess knowledge in the field of pediatric anesthesiology. This examination will be given under secure conditions in a computer-based format at Pearson VUE testing centers throughout the United States. Items for the examination are being developed by a committee composed of experienced pediatric anesthesiologists.
For further information, including the examination content outline, an examination tutorial, information about application and examination fees, and frequently asked questions, please visit the ABA website at www.theABA.org. ABA staff will also be available to answer any questions about certification or MOCA® at their exhibit booth at the SPA International Assembly of Pediatric Anesthesiology meeting in Washington, D.C., in October 2012.
Review of the Congenital Cardiac Anesthesia Society Meeting 2012
Morning Sessions
 By Wilson Chimbira, MBChB, FRCA
By Wilson Chimbira, MBChB, FRCA
Mott Children’s Hospital
University of Michigan Hospital and Health Systems
The Annual Meeting of the CCAS was introduced by President Dr. James DiNardo (Children’s Hospital Boston) who gave the opening remarks. Dr. Jumbo Williams (Stanford University) and Dr. Wanda Miller-Hance (Texas Children's Hospital) and the rest of the planning committee should be commended for putting on an excellent program.
The first session of the CCAS meeting was titled Oxygen: The Elixir of Life and Death and was moderated by Dr. Chandra Ramamoorthy (Lucile Packard Children’s). The first speaker was Dr. Francis X. McGowan Jr. (Medical University of South Carolina).He started off with a brilliant and stimulating basic science overview of the potential deleterious effects of oxygen therapy in a talk titled ‘Oxidative Stress and End Organ Injury’. He covered the pathways that lead to the production of reactive oxygen species (ROS) and reactive nitrogen species (RNS). The take home message was that depending on cell type both high and low oxygen tensions can lead to excess generation of toxic oxygen derived metabolites which can then lead to tissue damage. This may be even more profound in patients who have moderate chronic hypoxia/cyanosis which leads to a resetting of the hypoxia-normoxia setpoint. Dr. McGowan posed that they are even more susceptible to development of toxic oxygen derived metabolites at normal oxygen tensions which the tissues sense as hyperoxia. Dr. McGowan suggests caution after correcting a cyanotic lesion when separating cardiopulmonary bypass where patients may be exposed to higher oxygen concentrations that may lead to excess ROS production.
The next talk ’Supplemental Oxygen in the perinatal period: friend or foe’ was equally outstanding and it was delivered by Dr. Wally Carlo, a neonatologist (University of Alabama). He covered the history of supplemental oxygen on neonates in the perinatal period and then gave suggestions backed by the data on how we should manage these vulnerable patients. The American Academy of Pediatrics Neonatal Resuscitation Program recommends using room air during the initial resuscitation at birth in term infants and the use of 100% Oxygen only in infants who are bradycardic for more than 90 seconds. For preterm infants he recommends starting with 100% Oxygen and then titrating down to avoid hyperoxia. A study by Rabi et al in Pediatrics, 2011 showed an increase in persistent bradycardia in preterm infants that had been randomized to start with low oxygen concentrations titrated up (24%) compared to those starting at 100% titrated down(9%). He also covered two multicenter trials looking at target oxygen saturations in Premature Infants the SUPPORT trial out of the USA and the BOOST trial out of UK. The trials proposed that targeting lower oxygen saturation ranges between 85-89% compared with 91-95% would result in decreased incidence of severe Retinopathy of Prematurity (ROP) or death in preterm infants. However results showed a significant decrease in severe ROP but at the expense of an increase in death in the low saturation group. Dr. Carlo suggests targeting saturations of 91-95%.
The second session was moderated by Dr. Wanda C Miller-Hance (Texas Children’s Hospital) and was titled Emerging Technologies: Pulse Pressure Analysis and Non Invasive Cardiac Output Measurement. This session took on an international feel about it with the first speaker Dr. Maxime Cannesson (University of California Irvine). As an internationally recognized expert on hemodynamic monitoring we were fortunate to have him speak to us on Pulse Pressure Variation in Children: Past, Present and Future. However despite all the advances in adults in this area the pediatric population lags far behind largely due to a wide spectrum of ages, sizes, and weights. Secondly, the most commonly used technologies in adults are not yet designed for children. Thirdly, vascular access in children can be challenging and most hemodynamic monitors are not designed for this population. Finally, the cardiovasular physiology observed in children (especially in the pediatric cardiac intensive care unit) makes implementation of technologies extremely difficult.
Dynamic parameters of fluid responsiveness allow for accurate prediction of fluid responsiveness the most popular are derived from the arterial waveform ( pulse pressure variation, stroke volume variation). These parameters have been tested in several clinical studies in adults and have consistently been demonstrated as the best predictors of fluid responsiveness ( superior to central venous pressure or wedge pressure). Only a few studies have been performed in children so far and most of them seem to demonstrate that stroke volume variation is a strong predictor of fluid responsiveness while peripheral parameters such as pulse pressure variation and plethysmographic waveform variation fail to predict fluid responsiveness in this setting. It is important to note that stroke volume variation derived by Echo appears to be accurate but that derived from the arterial waveform may be impacted by arterial compliance and thus may be inaccurate.
The second speaker of the session was Dr. Katherine Taylor (Hospital for Sick Children, Toronto) representing our neighbors from north of the border. She discussed ‘Non invasive cardiac output (NI-CO) monitoring’ in children. Dr. Taylor has the distinct advantage of doing a lot of research on these various monitors and therefore provided a useful perspective on the various devices. The talk outlined what NI-CO monitors were available on the market, how they worked and their limitations. The NI-CO devices discussed included doppler devices, pulse pressure devices, impedence cardiography, partial Co2 rebreathing and pleth variability. The conclusion was that despite a lot of promise, most devices have very little evidence supporting their accuracy in pediatric populations and no evidence supporting a need to change patient management due to these devices.
The final session of the morning was more practical and was aptly titled ‘Sickest of the Sick, Non cardiac Surgery’ and was moderated by Dr. Helen Holtby (Hospital for Sick Children, Toronto). The presenters discussed three separate patients for operations that we as pediatric anesthesiologists would consider pretty routine however the patients themselves were not so straightforward. Dr. Scott Watkins (Vanderbilt University) presented a ‘Fontan patient presenting for posterior spinal fusion’. He discussed fontan physiology and its peri‐operative implications. He went on to cover the link between scoliosis and congenital heart disease and posed several theories for the link from possible embryonal association to the effects of the sternotomy on the stress loads in the spine. Finally he highlighted the unique challenges posed by the Fontan patient presenting for scoliosis surgery.
Dr. Mark Twite (Children’s Hospital of Colorado) covered I think the scariest case of the day ‘Pulmonary Hypertensive Crisis during Broviac catheter placement”. He covered the pathophysiology of pulmonary hypertension, presented some of the issues in the anesthetic management of a patient with pulmonary hypertension and management strategies to prevent and treat a pulmonary hypertensive crisis. The patient he presented was a patient with severe pulmonary hypertension on multiple pulmonary artery vasodilators. Dr. Twite discussed the effects of the commonly used anesthetic agents on pulmonary hemodynamics. He then went into great detail on various strategies to manage a pulmonary hypertensive crisis. He concluded with his goals for anesthesia in this case to avoid increases in PVR, maintain systemic BP and coronary perfusion and be prepared for a pulmonary hypertensive Crisis.
Dr. Peggy McNaull (UNC Children’s) presented the final case of the session ’Laparoscopic Nissen Fundoplication in a 3 month old s/p Norwood Procedure’. She reviewed the indications for a Nissen fundoplication and G‐tube in an infant with hypoplastic left heart syndrome s/p the Norwood Procedure. Dr. McNaull presented the outcomes observed in children with congenital heart disease after non cardiac surgery. She went on to review the physiologic effects of laparoscopic surgery on an infant with complex congenital heart disease and offered an anesthetic management plan.
Afternoon Sessions
 By Warwick A. Ames, MBBS
By Warwick A. Ames, MBBS
Duke University
The afternoon CCAS session, moderated by Dr. Courtney A. Hardy (Ann & Robert H. Lurie Children's Hospital of Chicago) began with the three best abstracts submitted and accepted to the 2012 CCAS.
Dr. Nicole Wilder (University of Michigan) presented her data suggesting that fluid overload can be used as a marker for poor outcome in neonates following cardiopulmonary bypass. Dr. Andrew D. Pitkin (University of Florida) presented his dynamic computerized model of single ventricle physiology, which permits the user to alter various parameters to understand how making those changes might alter the relationship between pulmonary and systemic blood flow. Finally Dr. Laura K. Diaz (Children’s Hospital of Philadelphia) retrospectively reviewed a detailed database to suggest that the cumulative exposure to volatile anesthetics, in children with congenital heart disease, had resulted in poor neurocognitive outcomes, most notably memory loss.
The following session, moderated by Dr. G.D Jumbo Williams (Lucile Packard Children’s), was the pro-con debate on the use of Recombinant factor VIIa. Dr. Williams introduced the debate with some background information. He noted that the drug is currently only approved by the FDA for uncontrolled bleeding in hemophilia patients, although the majority of its clinical use may be in pediatric cardiac surgery. A working group from the CCAS had previously been created to establish guidelines for it use. Upon questioning of the assembled audience, it seems to be use sparingly, as a rescue therapy, only after third round of products, at a dose 81-120mcg/kg, the dose recommended for hemophiliacs. A third of the audience had witnessed adverse events associated with its use.
Dr. Susan R. Staudt (Children’s Hospital of Wisconsin), speaking for the pro debate, acknowledged the limited FDA approval, and that 97% of use is ‘off label’. She briefly reviewed the mechanism of action, before examining the literature on efficacy. She noted very few randomized controlled trials had been published and that much of the data was from case reports. The largest study to date in children, by Pychinska-Pokorska, reported an 85% response rate and those in which it did not work, a surgical cause of bleeding was found. She accepted that another study by Ekert et al showed more bleeding with rVIIa but criticized the study for the inappropriate dosing, design and patient selection. Dr. Staudt considered the cost to be less than that of the potential blood products and time in the operating room. With regard to complications, she did not report a statistically significant increase in thrombosis, recognized that the study sizes were small, but asked the audience to consider the risks of continued hemorrhage.
The con argument, by Dr. Nina A. Guzzetta (Emory University) gave the audience five reality checks. Firstly that there are no RCT’s supporting the efficacy of rVIIa specifically in reducing bleeding post cardiopulmonary bypass in children. All other studies she noted were small and retrospective, including the supporting data presented by Dr Staudt. She presented new unpublished data suggesting that rVIIa does not increase thrombin formation above and beyond appropriate blood products.
Secondly that variable efficacy dosing has been noted in hemophiliac children versus adults, but there is simply no data on dosing in children with CHD. Thirdly, there is no accepted monitor for its efficacy. Pro-thrombin time cannot be used and when coagulant therapy was guided by thromboelastography, less rVIIa was likely to be used. In addition to stating the cost of the drug, Dr Guzzetta was concerned over the safety profile. She observed that it is a coagulant that could be triggered by activated tissue factor, present in abundance during CPB, sepsis etc, and therefore thrombosis should be anticipated. Indeed she sited several studies in children and adults reporting a 10% incidence of thrombosis.
Dr. Williams identified a change in practice where some institutions are giving rVIIa earlier to higher risk patients. The debate was concluded.
The following session was a disease update on the Borderline Left Ventricle (LV). The concept was introduced by Dr. Debra L. Kearney (Texas Children’s Hospital), a pediatric pathologist. Using an extraordinary photographic selection of pathological specimens, she described the spectrum of lesions associated with the hypoplastic left ventricle (HLH). She discussed the existence of the endocardial fibroelastosis (efe), a thickening of the endocardium with in the LV. She discussed the compressed LV of Shone syndrome and described the existence of the borderline HLV.
The next speaker was a pediatric cardiologist, Dr. Wayne Tworetsky (Children’s Hospital Boston). He discussed preventing the evolution of HLHS in utero by early detection, notably of critical aortic stenosis, and early intervention, including fetal surgery to open the aortic valve. He described how a variant of HLHS occurs with congenital diaphragmatic hernia, when the left heart is compressed creating a so-called hibernating left heart. He then introduced the concept of LV rehabilitation in patients with borderline HLV, with the ultimate aim of a bi-ventricle repair. This is an evolving technique, requiring refinement in patient selection, surgical techniques and critical care management. Anatomical and physiological aspects dictate the feasibility, in particular the presence of efe being a major limiting factor, along with valvular anatomy and function. It is unknown whether promoting a bi-ventricle repair will improve survival, long term outcomes and quality of life, over the current practice of a single ventricle repair for patients with HLHS.
The final speaker in this session was Dr. Sitaram Emani, a pediatric cardiac surgeon from Boston Children’s. Dr. Emani described the risk factors for bi-ventricular repair, notably small left structure, efe, presence of VSD and ventricular dysfunction, but that there was a group of children with borderline HLHS that were eligible. Typically these children would follow a single ventricle repair until after the glenn procedure, when the assessment of the ability of the left heart to grow would be made. He described the operative strategies that included efe resection, restriction of the ASD (to stress the LV) and repair of left sided valves. It seems again the cornerstone of LV rehabilitation is the presence of efe. Removing it is akin to peeling cartilage away, and it is made even more difficult with the close proximity of the conduction system to the endocardium and that the myocardium is thin. Once removed however improvement in systolic function is considerable.
He noted that left atrial hypertension is predictably a problem, especially in the first 48 hours. He concluded that LV salvage is possible after single ventricle palliation, requiring however multiple operations. Results of biventricular repair are acceptable at short term follow-up.
The final session of the meeting included a pediatric cardiac anesthesia version of Jeopardy, with audience participation. Coordinated by Dr. Anthony Clapcich and Dr. Radhika Dinavahi (Children’s Hospital of New York), the audience were exposed to a number of images and questions in what proved to be a fascinating and informative session.
Special Interest Group in Pediatric Pain Medicine Meeting Review
Morning
David M. Polaner, MD, FAAP
The Children's Hospital
The Special Interest Group in Pediatric Pain Medicine put together an impressive program at the winter 2012 SPA-AAP meeting. Dr. Anjana Kundu (Seattle Children’s Hospital) offered welcoming remarks and moderated the first session, which focused on the neurobiology and pharmacology of pediatric pain. Dr. K. Sunny Anand (St. Jude’s, Le Bonheur Children’s Hospital), one of the pioneers in the understanding of analgesics and pain in the neonate, spoke about the development of pain perception and processing in the neonate, the current understanding of how repeated painful stimuli (such as may occur in the NICU) may affect the longer term plasticity and development of pain pathways, and discussed the controversial and conflicting studies on the detrimental and potential neuroprotective effects of different analgesics on the developing brain. Term and preterm neonates are able to consciously process noxious stimuli, and imaging studies, EEG data and biochemical mediator data in both experimental animals and in humans show that perception is present, and hyperalgesia develops with repeated stimulation. Furthermore, in experimental animals, there is a decreased dose response to opioid analgesics, not related to mu receptor density or binding affinity, which occurs over time.
The NEOPAIN trial and its follow up studies, which looked at both neurological outcome and analgesic responses in neonates who received continuous morphine infusions, found some short term (hypotension, respiratory depression) and long term (short term memory, social function, adaptive behavior) adverse consequences in those neonates who received continuous infusions, although neuropsychological outcomes were similar. Anand also spoke about his recent work with ketamine, which, contrary to some other studies, suggests that it may be neuroprotective via NMDA receptor antagonism and an anti-inflammatory mechanism, and block excitotoxic cell death in a rat model. A pilot randomized controlled trial of ketamine prior to cardiopulmonary bypass suggests that this may occur in human neonates as well, with less glutamate release, lower choline and creatine levels and greater NIRS complexity in the treated vs. untreated group.
Dr. Sabine Kost-Byerly (Johns Hopkins) discussed a clinical problem that is increasingly well recognized as very common- tolerance to high dose opioids and sedative-hypnotic drugs in the ICU, weaning and abstinence syndrome. She first explained how and why tolerance develops, as down-regulation of opioid receptors, up-regulation of cAMP, and interaction with other pain mediating receptors, such as NMDA, lead to a chain of intracellular signal transduction that occurs largely independent of metabolic factors. Continuous receptor stimulation seems to be more problematic than intermittent stimulation, and short acting drugs with high receptor affinity are more problematic than longer acting drugs. She next discussed the difficulties in measuring withdrawal or abstinence syndrome, and how all of the scales, which are observational in nature fall somewhat short in specificity. Unfortunately, there are no clearly defined rules that can be easily implemented, other than the recognition that failure to wean requires the clinician to reassess and move to a lower dose more slowly. Most protocols are based on percentage reduction from the original or prior day’s dose, with the flexibility to move more slowly when clinical signs warrant.
The final speaker of the session was Dr. Senthil Sadhasivam (Cincinnati Children’s Hospital), who discussed using pharmacogenomics factors to personalize perioperative analgesic management. He first presented sobering data on the number and presumptive etiology of post-tonsillectomy deaths in the US – 18% were related to opioids alone, and only one half were related solely to surgery. At the same time, inadequate analgesia and serious side effects are reported in 50% of children receiving opioids after tonsillectomy. The genetic polymorphisms responsible for the enormous variability in opioid response range from variations in metabolism of codeine to methylmorphine (CYP2D6 and UGT2B7), variations in mu receptor-1 genes that can increase the effective analgesic dose of morphine four fold, and variation in COMT activity, decreased levels of which may increase both sensitivity to pain and the risk of developing a chronic pain syndrome.
These pharmacogenomic factors relate not only to analgesic efficacy itself, but also either predispose or protect against many of the opioid side effects, including respiratory depression. Because these are genetically determined, there are racial differences in drug effects, with Caucasians developing more side effects from morphine and African-Americans developing less, however, the African-Americans also had higher morphine clearance and received less effective analgesia.
Dr. Rosalie Tassone (University of Illinois at Chicago) introduced a session on the management of acute pain. First, Dr. Navil Sethna (Children's Hospital Boston) delivered a wide-ranging and comprehensive explanation of how meaningful analgesic management can be delivered. He integrated the basic science aspects of multi-modal analgesic strategies with the clinical delivery of those modalities to illustrate how to achieve optimal analgesia while minimizing untoward effects. He emphasized that one must chose meaningful measures and endpoints (e.g., effective analgesia with activity, not just at rest; return to daily activities; minimizing central sensitization, reducing metabolic and endocrine stress) in order to be successful. Finally he illustrated the theoretical and basic science points with data from several clinical investigations demonstrating the use of different modalities (opioids, central and peripheral neural blockade, non-opioid analgesics, gabapentanoids) and how those techniques could be used in combination to minimize side effects and increase analgesia.
Next, Dr. Tassone moderated a debate on whether standardized protocols should be the backbone of acute pain management. Dr. James J. Mooney (Seattle Children’s Hospital) took the “pro” position, arguing that protocol-driven care does not mean the same treatment regimen for all, but rather that both quality and efficacy are by nature driven by being able to measure what you do and being able to reproduce what you do for a given situation. Dr. Stephen R. Hays (Monroe Carroll Jr. Children’s/ Vanderbilt), arguing the “con” position, insisted that tailoring care to the individual was necessary to affect an optimal outcome in the real clinical world where no two patients respond exactly the same to a given intervention.
The morning finished with a panel discussion, moderated by Dr. Yuan-Chi Lin (Children’s Hospital Boston), and presented by Dr. Santhanam Suresh (Ann & Robert H. Lurie Children's Hospital of Chicago) and Dr. Alyssa A. Lebel (Children’s Hospital Boston) on the treatment of headache. The incidence of primary headache disorders in childhood is surprisingly high- 3-11% in children 3-11 years old and as high as 23% in pre-teens and teenagers, although in many of these children they are not recurrent. Migraine variants, including cyclic vomiting, paroxysmal torticollis and benign paroxysmal vertigo may be included in these numbers. The criteria for different headache syndromes were described, and the differential diagnosis discussed. Of note was the description of familial hemiplegic migraine, the first clearly defined genetic pediatric headache disorder. The therapeutic options, which are myriad, were discussed in detail, including the atypical anticonvulsants, triptans, antidepressants, beta blockers and conventional analgesics, as well as non-pharmacologic therapies.
Afternoon
Rita Agarwal, MD, FAAP
University of Colorado, Children’s Hospital Colorado
Session 4: Putting It All in Practice
Case Based Discussion on Managing Complex Pain Consults. Dr. Kenneth Goldschneider (Cincinnati Children’s Hospital) and Dr. Thomas Vetter (University of Alabama School of Medicine).
This was an interactive case based discussion that centered on several cases that had either been submitted by the audience or by the moderators. There was lots of discussion and questions raised unfortunately few good answers.
The first case was that of a 13 yo male with 15 month h/o “head pain” over L temple and variable distribution on blinded examination. He reported symptoms of pressure and pounding radiating down to his left mandible that were worsened with bending and laughing. His pain ranged from 10-10+/10. An extensive workup was mostly negative and multiple medication trials and cognitive behavioral treatments had failed to improve his symptoms. He was fully functional and only missed school for doctor’s appointments, He played on 3 basketball teams and mom was trying to get him accepted into a private school on a basketball scholarship. The topics discussed included treatment of atypical headache, when to stop investigations and how to handle family dynamics.
The next case was that of an 18 year old male s/p BMT now with severe graft versus host disease, including diarrhea, skin lesions and renal insufficiency with all over pain. He was admitted to the hospital for a GI bleed and severe abdominal pain. His family’s goal was to have him as alert and interactive as possible; his goal was relief of the pain. He was unable to take anything by mouth and had been on various PCA’s.
There were a number of excellent topics that were discussed including balancing the patient’s and the family’s goals, introducing the concept of palliative care during active treatment and the role of lidocaine or low dose ketamine infusions
The third case was a 15 y.o. healthy, normal girl with 2-3 year history of distal pain and GRAVITY-based discoloration of her feet/lower legs. If she stood or dangled her feet over the edge of a bed, her feet became dark and began to hurt. When she raised her legs, the pain dissipated pretty quickly, but not instantly, and not completely. Her hands and arms were also affected, but the pain was much less. There was NO swelling and no relationship to temperature. Her cap refill was really sluggish. This had halted many of her normal sports activities.
All her work-up had been negative. The next 2 cases were also on patients with extensive, expensive workups, one of whom had a diagnosis and one of whom did not. The common issues with all these cases were related to: how much and how long to continue testing, rules of engagement with the family and how to broach the clear need for psychology/psychiatry consult with the patient and family without alienating them.
This was a lively and extremely interactive session and although there were few answers, it was reassuring to know that even the most renowned pediatric pain practitioners were struggling with the same issues that many of the audience were.
The next lecture was by Dr. Rosalie Tassone (University of Illinois) on the topic of Can We Prevent Chronic Pain? The answer to the question posed in the title was a succinct “NO”. She presented the natural history and prevalence of pain based on the scant available literature. Estimates of the prevalence of chronic pain range from 10.1% to 55% in adult studies and 8% in pediatric studies. Increasing age, female gender, lower socioeconomic status, chronic abdominal pain and cancer all increase the risk of developing chronic pain. Thoracotomy, hernia repair, amputation, pyloromyotomy, and multiple surgical procedures are all associated with an increased incidence of postoperative pain.
Unfortunately, there is very little good data to support treatment to prevent chronic pain. Regional anesthesia has been used successfully to decrease the incidence of phantom limb pain after amputation and in patients with peripheral vascular disease. Low dose ketamine may decrease the incidence of chronic pain after total hip arthroplasty, and possibly spine and thoracic surgery. The use of alpha 2 agonists has been advocated, but there is even less evidence supporting their utility in preventing chronic post-operative pain.
Neuroimaging and Brain Plasticity in “Strange” Pain Disorders by Drs Alyssa Lebel (Children’s Hospital Boston) and Charles Berde (Massachusetts General Hospital) was an incredibly fascinating and exciting look at the future. It is impossible to do the talk justice because of the impact of the slides and visual images of brain differences in patients with and without pain, or before and after treatment. Common denominators for “strange pain syndromes” is that they do not have a dermatomal distribution, good animal models do not exist, they have inconsistent or negative responses to analgesics and inconsistent or no response to numbing the area of pain. Psychological factors probably pay a role in perpetuating and exacerbating the pain, but do not cause it.
Successful treatment usually requires a combined approach that includes psychological rehabilitation. There appears to be a distortion in the brain’s sensory and motor maps that can be changed with appropriate therapy. fMRI, PET scans and MEG all show a distortion in the homunculus. Chronic pain can lead to areas of cortical thinning in specific areas of the brain which may represent neural tissue loss. These areas of volume loss normalize once the pain resolves. Dr Lebel has documented this in children with CRPS. I would strongly recommend that people who are interested in this type of imaging review Drs Berde and Lebels spectacular handout on the SPA website.
Perioperative Considerations for the patient with Chronic Pain by Dr. Jeffrey Koh (Doernbecher Children’s) was the last lecture of the session and an excellent review of treating the chronic pain patient who has to come to the OR. There is good evidence that patients with chronic pain do have a greater need for opioids in the post-operative period and take longer to recover from their pain. This may be due to several factors including central or peripheral hypersensitivity, opioid tolerance. Opioid induced hyperalgesia and previously undertreated or under recognized pain.
It becomes increasing important in these patients to fully explore non-opioid options and to be aware of possible drug interactions (prolonged QT with methadone and with TCA antidepressants). Recommendations from Dr Koh were to consider the use of longer acting opioids and to expect that these patients may require double the dose that opioid naïve patients would. The patients’ baseline opioid requirements MUST be considered and accounted for.
There are at least 2 good studies that have found gabapentin to decrease the use of post-operative opioids with minimal side effects. Ketamine has also been used with good results, however doses and dose ranges range anywhere from no bolus, 1mg/kg bolus, no infusion of infusions of 1-10ug/kg/minute. Both clonidine and dexmedetomidine have been shown to help decrease post-operative analgesic requirements. NSAIDs have opioid sparing effects, but in some situations can increase bleeding. Regional should be used as much as possible. The key however to managing these often complex patients is good planning and communications with the patient, family and other health care providers.
CRNA/AA/NP Special Interest Group
 By Paula J. Belson, CRNA
By Paula J. Belson, CRNA
Children's Hospital of Los Angeles
The CRNA/AA/NP SIG meeting occurred on Friday afternoon during the 2012 Pediatric Anesthesiology meeting at the Marriott Tampa Waterside Hotel. We had 11 CRNAs, 4 AAs, 1 NP, 2 nursing students, and 1 MD attend the meeting. This was quite a step up from our previous two meetings with approximately 5-6 CRNAs in attendance. Expanding the group to include Anesthesia Assistants and Nurse Practitioners in order to include all those who are active participants in anesthesia care for children was welcomed by all. The main purpose of the group is to meet in an informal environment within the SPA meeting and support the educational accomplishments of colleagues, while also allowing open discussion of anesthetic techniques and any other issues regarding pediatric anesthesia care.
We started the meeting with a brief welcome and encouraging words from Dr. Lynn Martin (Seattle Children’s Hospital), current SPA president. Paula Belson, CRNA (Children’s Hospital, Los Angeles) then explained to new attendees the history of the last two years of the SIG meeting and the future goals of the SIG. Last year’s goal of encouraging attendance and participation was achieved by distributing email invitation flyers to all CRNAs, AAs, and NPs registered for the meeting and by mass email introduction of the group sent to the chairs of the departments at all pediatric hospitals affiliated with SPA.
A brief introduction of the AAs was given by John Ng (Children's Hospital, Colorado). He also introduced to the group the Committee on Pediatric Anesthesia (CPA) which is an anesthesia subspecialty committee of the American Academy of Anesthesiologist Assistants. Dr. Robert Greenberg (Johns Hopkins Children’s Center) welcomed all and invited us to participate on the pediatric anesthesiology discussion group through Hopkins as an additional way to communicate with anesthesia colleagues across the country.
We had two scholarly presentations. The first one was by Jamie Furstein, CRNA, DNAP (Cincinnati Children’s Hospital). He presented a poster presentation from the ASA Annual Meeting last October on a case study where dexmedetomidine was used as the primary anesthetic for a laryngoscopy and bronchoscopy in a child with a precarious airway. Jamie has also had an article published in the AANA Journal (October 2011) titled, “Use of Dexmedetomidine for Monitored Anesthesia Care for Diskography in Adolescents.”
Then second presentation was given by Katrin Sames, CRNA, DNAP (Children’s Hospital at Vanderbilt). She presented a Powerpoint presentation on "Proper shielding techniques and protection of pediatric patients from diagnostic radiation exposures" which was her capstone project for her recently completed DNAP. A discussion regarding how individual institutions shield their patients from radiological exposure followed.
Future goals for the group are to promote education and research among the various members of the pediatric anesthesia care team, encourage attendance and participation at SPA, and identify ways we as CRNAs, AAs, and NPs can actively contribute to the field of pediatric anesthesia. We encourage all CRNAs, AAs and NPs to join us next year in Las Vegas!
Pediatric Anesthesiology 2012 Meeting Reviews
Session 1: Disaster and Trauma
Reviewed by Cheryl K. Gooden, MD
Mount Sinai Medical Center
The first morning session moderated by Dr. Donald (Hal) Shaffner, Jr. (Johns Hopkins Hospital) provided an overview of neurologic injury, trauma and shock and their respective management. Indeed, there is some overlap in the presentation and management of the pediatric and adult neurotrauma patient. However, much of this session focused on the unique features observed in pediatrics.
Dr. Monica Vavilala (Harborview Medical Center) presented “Management of Traumatic Brain Injury in the Pediatric Patient.” She began by highlighting statistics related to pediatric trauma in the USA. For example, a case of severe pediatric trauma occurs every six to nine minutes. Traumatic brain injury (TBI) remains the leading cause of overall death in children over the age of one year. The incidence of mortality from TBI among pediatric patients is 2.5 – 12%. In fact, when comparing TBI in the child vs. the adult, the pediatric patient is more susceptible to this type of injury. There are several reasons for this finding and include the larger head to body ratio, immature cranial bone and neural tissue formation.
Dr. Vavilala provided a concise review of cerebral physiology and pathophysiology. She pointed out that in children the cerebral blood flow (CBF) changes with age and possible gender differences may be observed. Of note, children with impaired cerebral autoregulation occurring early after TBI may experience poor long term outcome. Therefore, early assessment and treatment of these patients is important.
The remainder of Dr. Vavilala’s presentation dealt with the clinical management of the child with TBI. Care of the patient with TBI should begin with the primary and secondary surveys. Immediately following the performance of these surveys the definitive care begins. For further information on definitive care she recommended the 2003 Brain Trauma Foundation Guidelines.
Dr. Stefan Parent (Hôpital Ste-Justine, Montréal) presented “Perioperative Management of Acute Spinal Cord Injury in Children.” Much of his presentation focused on the unique features of spinal cord injury in children from the perspective of a pediatric orthopedic surgeon and researcher. In addition, he reviewed current treatment options for spinal cord injury.
Spinal Cord Injury (SCI) in the pediatric population is relatively rare but the occurrence has a significant psychological and physiological impact. Dr. Parent alluded to the fact that the mechanism of injury, the male-to-female ratio, and the level of injury in the child differs from that of the adult. These factors play an important role in the management of these patients with SCI.
The association between motor vehicle accidents (MVA) and the younger child was more common when compared with the adolescent. On the contrary, the adolescent was injured more often during sporting activities. All-terrain vehicles (ATVs) are responsible for a higher rate of injury in children than in adults. He highlighted the fact that a large predominance of SCI was observed in males compared to females. In addition, it is more common for children to have a higher level of cervical injury compared to adults.
Dr. Parent reminded us that spinal cord injury without radiological anomaly (SCIWORA) remains a recognized entity in the pediatric population. Therefore, a high index of suspicion for SCIWORA is necessary with the assessment and evaluation of sports injuries and other related injuries. It cannot be emphasized enough that physical examination has an important role in SCI.
He concluded his presentation first with there being a paucity of evidence-based medicine to support the use of steroids and hypothermia in SCI, and should not be routinely used. Next, the presence of significant cervical injury cannot be excluded on the basis of absent radiological anomaly. Finally, there is some evidence in the literature to suggest that neurological recovery may be better in children than adults with SCI.
The final speaker in this session was Dr. Richard Dutton (Anesthesia Quality Institute, Park Ridge, IL) who presented “Hemorrhagic Shock in the Pediatric Patient: New Therapies and Practices.” Dr. Dutton began by presenting several trauma case scenarios. He followed with an overview of the evolution of fluid resuscitation from World War I to the present, in the presence of hemorrhage. Much of the science behind fluid resuscitation is based on studies in the adult population. The majority of this information has been extrapolated to pediatrics.
Based on the evidence, Dr. Dutton indicated that the preferred management for hemodynamically unstable hemorrhaging patients is blood products (RBC, plasma, platelets) instead of crystalloids or colloids. The guiding principle is not to give a solution that doesn’t promote clotting or carry oxygen.
Dr. Dutton summarized his remarks with the following recommendations:
- Maintain systolic blood pressure 80 – 100 mmHg
- Maintain functional blood composition, using empiric 1:1:1 transfusion therapy
- Maintain normal serum ionized calcium
- Maintain core temperature >35°C
- Follow base deficit and serum lactate as markers for hypoperfusion
- Transition the patient to deep anesthesia
Session 2: News You Can Use
Elizabeth S. Yun, MD
University of Wisconsin Hospitals and Clinics
Four speakers presented updates on patient initiatives in pediatric anesthesiology
The first speaker Dr. Donald Tyler (Children’s Hospital of Philadelphia) and the executive director of Wake Up Safe, the Pediatric Anesthesia Quality Improvement Initiative, presented a history and update of this program. Wake Up Safe was started 5-6 years ago to create a registry for reporting and analyzing adverse events. The resulting information would then provided a basis for proposing improvement initiatives. Setting up the program required funding from participation institutions and the APSF, finding the right data management system, and taking care of legal issues of confidentiality and IRB.
As of this time, 15 institutions around the country are participating in this program. The most prominent events reported are wrong side procedures, syringe swaps and hyperkalemia related cardiac arrest. Of these, medication errors account for 17% of all cases reported, with administration of incorrect doses being the most common error. occur with infusions due to incorrect infusion pump programming. Of those administering medications, attending physicians had the highest rate of error. Fortunately most medication errors do not lead to any actual harm to the patient.
With this data, the members of this program are working on an initiative to decrease medication errors by creating ways of collecting data on drug labeling, standardization of infusion pump programs, mitigation of human factors, and verification of drug and drug concentrations. In the future, this program will continue to collect and analyze reports, expand the QI initiative and encourage other institutions to participate. More information on this program can be found on the SPA website, www.pedsanesthesia.org and questions can be sent to wakeupsafe@gmail.com
The second speaker, Dr. David Polaner (Children’s Hospital of Colorado), discussed the Pediatric Regional Anesthesia Network. This project started as a research network and highly audited case registry supported by the SPA and participating institutions, and endorsed by the AAP section of Anesthesiology and Pain Management. Participants collect data on every regional anesthetic performed on patients 18 years and younger. The data is entered over a secure internet connection to a central database and is carefully audited for accuracy.
As of January of 2012, 36,000 cases have been entered. Findings with the first cohort of 14,517 blocks on 13,725 patients showed no deaths, and the rate of complications and adverse events was similar to the European data, with catheter issues of kinking, dislodgement, or malfunction being the most common. No deep infections have been noted. Dural puncture occurred in 9 out of 1000 cases with 4 out of 26 patients developing PDPH requiring a blood patch. While there were episodes of respiratory depression, no arrests occurred. No issues with local anesthetic toxicity and permanent nerve injury were noted. In the future, the program continues to seek participants to expand the network and increase the database. With this database, anesthesia departments will be able to use the findings to help with quality improvement in pediatric regional anesthesia and as benchmark data for their practices. If interested in more information, please contact David Polaner david.polaner@childrenscolorado.org or Christie Wolf, the project manager at christiew@axioresearch.com
The third speaker, Dr. Joseph Cravero (Dartmouth Hitchcock Medical Center), reviewed some findings of the Pediatric Sedation Research Consortium. Over 30 institutions participate in this consortium ranging from free standing children’s hospitals to community hospitals. Each institution has a PI responsible for collecting data that is then entered on a web-based tool and de-identified. Participating physicians come from a variety of specialties including anesthesiology, emergency medicine, intensivists and hospitalists. Each institution receives quarterly reports on its own data but not on other participants. Over the years, the database has provided the data for multiple studies on pediatric sedation issues.
In terms of unplanned treatments during sedation, 1 in 100 cases have involved major airway interventions, the most common being positive pressure bag mask airway. Based on this finding, a core competency for providing sedation is the ability to provide positive pressure ventilation. The data indicate that many different providers use propofol. While the morbidity and mortality are low, many complications are associated with airway obstruction, laryngospasm, stridor wheezing and central apnea. These data suggested a need to credential core competencies for propofol sedation. Another study based on the data showed that there wasn’t a large difference in rate of complications across specialties if the sedation providers were part of an organized sedation service. Among obese patients, there was an increased incidence of airway obstruction and unexpected need for bag mask ventilation and secretions.
The data has also been used to study how pediatric patients are monitored during sedation. It appears that while 95% of patients are monitored by pulse oximetry, only 63% have pulse oximetry, ECG and intermittent BP monitoring. Out of all groups, anesthesiologists were the most likely to use ETCO2 monitoring. Based on this work, the consortium’s future plans include more focused data collection, more multicenter observational or randomized studies on specific issues and to find ways of improving quality of care through these research endeavors.
The final speaker was Dr. Nancy Glass (Texas Children’s Hospital) who presented Sedation Disasters Outside the Hospital: How Can We Impact Outcomes? She stated that there is no data for patients receiving sedation from non-anesthesiology providers in clinics outside of the hospital. Most information about adverse outcomes in clinics is anecdotal and is found on such websites as http://www.teethremoval.com/dental_deaths.html or by using Google to search for dental deaths. The reasons for these bad outcomes include overdose, inappropriate use of agents, no monitoring or physician presence, no personnel for post sedation observation, failure to recognize the problem and improper patient selection. These events can happen in any setting regardless of the health of the child. As pediatric anesthesiologists we can partner with the American Academy of Pediatric Dentistry and other specialties to provide guidelines and resources. We need to advocate at the state level for legislation to protect patients and we need to educate parents and families about the risks.
AAP Advocacy Lecture: Disaster and Humanitarian Response, Kids are Still Different
By Allison Kinder Ross, MD
Duke University
As per prior SPA meetings, the AAP Advocacy Lecture always promises to entertain by presenting issues that are outside of the normal realm of a meeting on pediatric anesthesia. This year was no different as Dana Braner, MD, FAAP, FCCM (Oregon Health and Sciences University) spoke on the topic of the care of children in the face of disaster. He began his talk by presenting recent history of disasters and the lack of preparedness that existed with the sudden onset and large scope of destruction. Video footage of earthquakes and the resulting tsunamis that occurred revealed the vulnerability of society. As an example of the effects of disaster on children, two thirds of the deaths in the 2004 tsunami were children.
To illustrate the lack of preparedness, only 16% of Americans surveyed felt that they were prepared for a large-scale disaster. However, 43% felt that they were not at risk when, in fact, 91% of Americans live in areas where there is moderate to high risk of a large-scale disaster. These disasters not only include natural disasters but also pandemics such as the pandemic flu, and terrorism including school shootings that are specifically targeted at children. In the United States, there have been 1700 disaster declarations by the President in the past 25 years.
The definition of disaster is any event that overwhelms available resources. It can be widespread or concentrated, but it affects the young, the old and the infirmed disproportionately. The four phases of disaster are mitigation, preparedness, response and recovery. One design does not fit all, and the needs of children are rarely taken into account. The challenges with preparedness for disaster for children include their unique physiology, they require caregivers, they have developmental issues, and there are deficiencies in the 4 “S’s” (space, stuff, staff, system). The physiologic issues that result in difficulties center around the facts that children may be more susceptible to injuries and adult medications and equipment are not suitable. There is no standardized triage system for children despite that they are more likely to respond to timely care. It must also be emphasized that to care for a child, the caregiver must also be cared for.
The Institute of Medicine (IOM) found that only 6% of all emergency rooms have the necessary supplies to take care of all ages of children, and only half of all hospitals are equipped to do so. In addition, skills required to take care of a child will deteriorate in staff that do not take care of children routinely. The summary of the IOM’s findings were that emergency departments and EMS systems overall were unprepared to manage a pediatric disaster.
In 2010, the “National Commission on Children and Disasters Report to the President and Congress” made several points on the issues at hand. Children account for one third of the population but only one tenth of all ICU beds are pediatric. Prior work in adults had occurred and was published in CHEST in 2007 by the Task Force on Mass Casualty Critical Care. There was only one pediatrician on the task force and the recommendations were mostly not applicable to children. They determined that the complexity of care of the child was not appreciated and that a separate task force would be needed.
This task force, the Pediatric Emergency Mass Critical Care (PEMCC), is comprised of 35 experts and they presented recommendations with regard to stockpiling equipment, medications, rules for use of these as well as the use of conversion charts and length/weight estimates. Additional recommendations were that every hospital with pediatric or neonatal ICUs should prepare for disaster. The purpose of making ICUs prepare for disaster patients is supported by history where there was a 45% mortality in make-shift ICUs in disaster zones. The thought is to take the ventilated ICU children and put them in wards, take ward children and put them in the make-shift areas such as gymnasiums and cafeterias, and use the ICUs for the sickest disaster patients. This “Critical Care Surge” essentially turns an entire hospital into an ICU. Triage, of course, is an essential component, and a severe pandemic is still not thought to be able to be accommodated even with these provisions.
In conclusion, Dr. Braner recommended that all pediatric providers should advocate for the needs of children in disaster preparedness and be prepared to participate if such an event occurs. The PEMCC is important, and pediatric anesthesiologists are an essential part of the process.
Recommended reference:
Deliberations and recommendations of the
Pediatric Emergency Mass Critical Care Task
Force: Executive summary
Niranjan Kissoon, MD, FRCP(C), FAAP, FCCM, FACPE; for the Task Force
for Pediatric Emergency Mass Critical Care
(Pediatr Crit Care Med 2011; 12[Suppl.]:S103–S108)
The AAP Robert M. Smith Presentation
By Allison Kinder Ross, MD
Duke University
Dr. Constance Houck (Children’s Hospital Boston) represented the AAP as the presenter of the AAP Robert M. Smith Award to Dr. Nishan “Nick” Goudsouzian. After a brief introduction to the origins of the award, Dr. John Ryan (Children’s Hospital Boston) introduced the recipient by way of video.
Dr. Ryan shared stories of Dr. Goudsouzian and relayed the smoothness by which the award recipient performed his clinical care and how he provided a sense of stability and wellbeing when he was in charge. Dr. Ryan also touted Dr. Goudsouzian’s impressive academic success by listing the numerous books, chapters and articles that he had published in his career. At the completion of the video introduction, Dr. Goudsouzian took the podium in the presence of a standing ovation from the attendees. He shared with the audience the history of Dr. Smith and some of their past experiences.
Dr. Goudsouzian relayed the message that he hoped to continue Dr. Smith’s legacy that “to take care of the child” was always the most important mission.
Saturday Morning Session
By Chris Glover, MD
Texas Children’s Hospital
This review covers Saturday’s first morning session moderated by Dr. James Dinardo (Children’s Hospital Boston). Dr. James Fehr (St. Louis Children’s) started the day covering fragile hemoglobinopathies. The primary emphasis was placed on sickle cell disease which is one of the most commonly inherited genetic diseases. Time was also spent covering hereditary spherocytosis and thalassemias. Sobering sickle cell (SC) statistics presented included a mortality rate approaching 20% in those reaching 8 years of age in Kenya. Asthma exacerbation leading to SC crises results in mortality rates approaching 50% in those reaching 40 years of age.
Dr. Fehr reported the relatively wide variation that can occur with fluid management and transfusion triggers when it comes to these chronically ill patients; further demonstrated by audience participation on managing a wide variety of patients and procedures. Dr. Fehr then transitioned to emphasize principles that should be incorporated into practice perioperatively.
Recommendations included
- Avoidance of hypotension and hypothermia
- Avoidance of hypoxemia and acidosis
- Appropriate fluid administration
- Proper and multimodal analgesia
- Emphasis on appropriate communication between the services involved in care perioperatively (surgery, anesthesiology, hematology, family, and patient)
A brief discussion was held on the associated signs and symptoms of thalassemia and hereditary spherocytosis. Common manifestations from these disorders (fatigue, poor growth, hepatosplenomegaly) relate to the hemolytic anemia that is commonly seen with these disorders.
Dr. Blaine Easley (Texas Children’s Hospital) covered the disturbing increased trend of venous thromboembolus (VTE) in the pediatric population. This increase has been noted in all age groups and approaches 100% amongst all age groups over a 6 year span (2001-2007).
The most common risk factors for thrombosis include:
- Central Line
- Sepsis
- Immobility
- Malignancy
- Surgery
The presence of one of the risk factors placed VTE risk at >50%. Malignancy was the associated condition noted to be most causal for recurrent VTE. An interesting note by Dr. Easley reported that the incidence of venous thromboembolus was independent of catheter type, catheter size, or duration of placement. Direct mortality approached 2% in studies out of the UK (Pediatrics 2009, 124:1001-1008) and Canada (Pediatric Research 2000, 47:763-766).
Therapeutic options for VTE include thrombectomy and thrombolysis. A new recommendation via placement of an IVC filter was recommended in those greater than 10 kg. Another option includes LMWH for 5 days followed by Vit K antagonist treatment for 6-12 months.
Recommendations to decrease this issue were to start prophylaxis in those patients on long term TPN using a vitamin K antagonist, to form a pediatric coagulation service, and to be mindful of special populations (congenital heart, oncology, pediatric trauma) that may need interventions. Risk stratification of patients and the appropriate therapy were covered eloquently in the chart cited below.
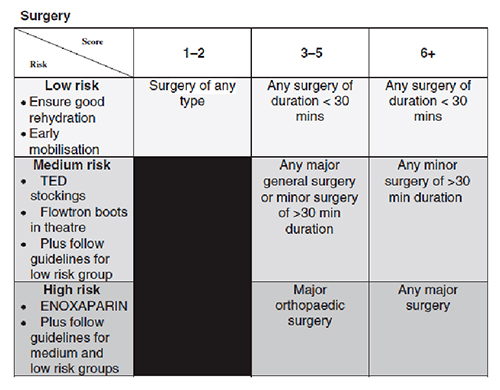
Dr. G.D. “Jumbo” Williams (Lucile Packard Children’s) discussed perioperative management of bleeding dyscrasias and coagulopathies. While it is important to be cognizant of the multitude of bleeding dyscrasias that exist, Dr. Williams stressed the vast majority (>95%) of the coagulopathies encountered are the hemophilias (A&B) and Von Willebrand’s disease. Screening tests (PT, PTT, INR) commonly thought by us to be useful are oftentimes poor predictors of potential perioperative blood loss. A detailed bleeding history however, is far more predictive of bleeding risk.
Thrombocytopenia was also discussed as and Dr. Williams pointedly mentioned risk approaching 20% in those with platelet counts ranging from 10-99. A synopsis of treatment is to initiate transfusion of platelets when the platelet count is less than 50.
Massive transfusion in the face of trauma was also discussed by Dr. Williams. INR is the best predictor as an outcome measure in trauma for assessment of coagulation.
While IV bolus dosing is the standard for volume repletion, fibrinolysis will be increased as hemodilution results in dilution of coagulation factors while clot strength remains unchanged. Treatment options include
- Antifibrinolytics
- Desmopressin
- blood components
- factor replacement.
Recommendations for therapy include giving prophylactic antifibrinolytics. Dr. Williams did set a target ratio for FFP and blood - FFP/PRBC 1:2 to 1:1. Platelet counts should be greater than 100000 with fibrinogen at 1.5-3.0. The message of this talk was understanding the importance on the potential etiology of coagulopathies seen, so we can know the best approach to treat it.
Saturday Oral Presentation
By Elizabeth M. Yun, MD
University of Wisconsin Hospitals and Clinics
On Saturday afternoon, five investigators presented their research as part of the AAP/SPA Abstract Awards.
The first investigator, Dr. Christopher Ward (Cinncinnati Children’s Hospital), presented Vulnerability to Anesthetic Induced Neuroapoptosis is Determined by the Maturational Age of the Cell and not the Age of the Animal. This study tested the hypothesis that cell age and maturational stage of the neuron determine anesthetic induced apoptosis instead of the age of the animal. The experiment involved two groups of 21 day old mice, one group that was exposed to room air and the other to 6 hours of isoflurane anesthesia. Newborn mice were also injected with BrdU, a thymidine analog, to birthdate the neurons at 4 different times prior to anesthesia exposure. The brain tissue was then immunostained for BrdU and capsase 3, a marker of apoptosis. The results showed that anesthetic exposure at day 21 led to an increase in neuroapoptosis at the dendate gyrus. Cells younger than 15 days were the most vulnerable and that the apoptotic neurons were identified as immature post mitotic granule cells. These findings suggest that anesthesia neurotoxicity may be related to the stages of neuronal maturation.
The second presentation was Racial Difference: Impact on Morphine Clearance and Perioperative Pain in Children by Dr. Pornswan Ngamprasertwong (Cincinnati Children’s Hospital). This study noted that African American and Caucasian pediatric patients have a different analgesic response to morphine. In a prospective genotype blinded experiment, both groups received 0.2 mg of morphine for tonsillectomy surgery. Serial blood samples for morphine, morphine-3-glucuronide and morphine-6-glucuronide levels were drawn. Additionally UGT2B7, the major Uridine Glucuronyl Transferase isoform responsible for 3- and 6-glucoronidation of morphine, was tested for genotype. The results showed that African American patients had a higher clearance for morphine compared to Caucasian patients. However, even though African American patients had more of the wild type UGT2B7 isozyme,common UGT2B7 genetic variations were not associated with observed racial differences in morphine clearance.
The third presentation was Effect of Vasopressor Selection on Cerebral Blood Flow and Intracranial Pressure in a Swine Model of Pediatric Critical Care by Dr. Benjamin Bruins (Children’s Hospital of Philadelphia). Many large animal models for studying traumatic brain injury utilize volatile anesthetics. However, volatile anesthetics alter the cerebrovascular response of the brain. Consequently, the results of those studies may not translate well to humans. This study used a new sedation model based on a common pediatric ICU sedation plan and examined the effects of several vasopressors on cerebral blood flow(CBF), mean arterial pressure (MAP) and intracranial pressure (ICP). Four week old, nontraumatized piglets were anesthetized and then sedated with intravenous infusions of fentanyl and midazolam. They were then randomly exposed to vasopressin, phenylephrine and norepinephrine and the effects on the above variables measured. Only norepinephrine increased MAP with increased dose. ICP and CBF levels did not increase with any of the vasopressors. Based on this work, this sedation model will be used to assess cerebrovascular hemodynamics and the neuroprotective effects of vasopressors in traumatic brain injury.
Dr. Angela Cambic (Children’s Memorial) presented Pharmacokinetics of Bupivacaine Following Femoral and Popliteal Nerve Blocks with Subsequent Continuous Femoral Nerve Catheter Infusions for Adolescents Undergoing Anterior Cruciate Ligament (ACL) Repair. This study is the first to address the steady state pK of bupivacaine used in continuous femoral catheter infusion in adolescents. In this work, adolescents undergoing ACL reconstruction received femoral and popliteal nerve blocks 0.25% bupivacaine at the start of surgery followed by a femoral nerve catheter with a continuous infusion 0.1% bupivacaine at 4 ml/hr that was started in the post anesthesia care unit (PACU). Bupivacaine levels were measured 5, 15, 30, 60, 120 minutes in the hospital and at 24 and 48 hours by a fingerstick sample done by the patient. The results showed that the steady state level of bupivacaine remained below the toxic level even after 48 hours of a continuous infusion. Another important aspect of this study was the use of a fingerstick for measurements.
The final presentation was Inhalational Induction with Vasoparalytic Sevoflurane: Are we Hyperoxygenating while Anesthetizing Developing Brains? by Dr. Jaspreet Sangha (Children’s Hospital of Michigan). As the study noted, cerebral hyperoxia may be a contributing factor in neuroapoptosis, induction of pro-inflammatory cytokines, and inhibition of growth factor signaling cascades. Using sevoflurane may lead to cerebral hyperoxia because of its cerebral vasodilatory properties. In this retrospective review, data from patients who had INVOS® Cerebral/Somatic Oximeter for noncardiac surgery was collected. Patients received either a high dose sevoflurane induction or a propofol induction. Maintenance of anesthesia remained the same with 1.5% isoflurane, air and oxygen mix for and FiO2 of 33%. Changes in the cerebral oximetry levels from baseline were examined from the time of induction to one hour into surgery and compared between the two different anesthetics. The results showed that an 8% sevoflurane induction had a significantly marked increase in cerebral hyperoxia levels compared to propofol induction.
Sunday morning: Editors’ Picks
By Anuradha Patel, MD
New Jersey Medical School
This is one of my favorite sessions at the SPA/AAP winter meeting. The editors or editorial board members from three prominent journals discuss articles that were worth reading in their opinion. The session started with Dr. Lance Lichtor (UMass Memorial) from the Editorial Board of Anesthesiology. He talked about the site http://pg2a.org started last year, Anesthesiology’s blog for education and more.
He discussed the following five papers on various topics from Anesthesiology 2011
1. Case scenario: perianesthetic management of laryngospasm in children. Orliaguet GA, Gall O, Savoldelli GL, Couloigner V. Anesthesiol 2012; 116:458-71.
Case scenario based review of management of laryngospasm in children. The paper discusses the “laryngospasm notch” which was first described by Larson in 1998. The area is a triangle located behind the earlobe, formed by the base of the skull, the mastoid process and ramus of the mandible. The index and middle fingers are place in the notch and pressure applied in a medial and cephalad direction, the airway is opened by sliding the mandible forward. There was input from the audience that this maneuver is used by many in their clinical practice, they were unfamiliar with the name.
2. Changing healthcare providers' behavior during pediatric inductions with an empirically based intervention. Martin SR, Chorney JM, Tan ET, Fortier MA et al, Anesthesiol 2011; 115:18-27.
These investigators have used a novel approach to management of preoperative anxiety in children. Healthcare providers (HCP) were trained with an empirically derived intervention, (Provider-Tailored Intervention for Perioperative Stress) to increase behaviors that promote children's coping and decrease behaviors that may exacerbate children's distress. The intervention successfully modified HCP and parent behaviors.
3. Pediatric surgery and parental smoking behavior. Shi Y, Warner DO. Anesthesiol 2011; 115:12-7.
This study determined if there is an association between children undergoing a surgical procedure and changes in their parents' smoking behavior. Survey data from the National Health Interview Survey was analyzed and included 9,289 parent respondents who provided information on both themselves and their children. The conclusion was that parents who smoke were more likely to make a quit attempt within the past 12 months if their children had surgery within this time, but they were not more likely to succeed in maintaining abstinence and thus could benefit from assistance.
4. Identical de novo mutation in the type 1 ryanodine receptor gene associated with fatal, stress-induced malignant hyperthermia in two unrelated families. Groom L, Muldoon SM, Tang ZZ, Brandom et al. Anesthesiol 2011; 115:938-45
Increasing evidence indicates that a subset of individuals with MHS develop MH-like symptoms during exercise, emotional stress, exposure to environmental heat stress, or a combination of these triggers. Clinical histories and specimens from two children who died of non-anesthetic awake events were studied. Both patients had no family history of MH or other neuromuscular disorders, but the patients did have low muscle tone. The first patient experienced an anesthetic event suspicious for MH, followed by numerous awake episodes with MH like symptoms. He had a markedly positive caffeine-halothane contracture test and was placed on low dose prophylactic dantrolene, but died at age nine during a fulminant episode. The second patient experienced a previous awake episode in the absence of anesthesia, presented to the ER with an MH like episode, the body temperature reached 108 degrees and she died despite receiving dantrolene 10mg/kg. Examination of the type 1 ryanodine receptor gene revealed the presence of an identical new variant in both and a second unique variant in one. The take home message is that sporadic cases of MH due to de novo mutations in the RYR1 gene are likely to be more common than previously appreciated.
5. Neonatal desflurane exposure induces more robust neuroapoptosis than do isoflurane and sevoflurane and impairs working memory. Kodama M, Satoh Y, Otsubo Y, et al. Anesthesiol 2011; 115:979-91.
Six-day-old mice were exposed to equivalent doses of desflurane, sevoflurane, or isoflurane for 3 or 6 h. Neonatal exposure to desflurane induced neuroapoptosis with an anatomic pattern similar to that of sevoflurane or isoflurane; however, desflurane induced significantly greater levels of neuroapoptosis than almost equivalent doses of sevoflurane or isoflurane. In adulthood, mice treated with these anesthetics had impaired long-term memory.
Dr. Peter Davis (Children’s Hospital of Pittsburgh), section editor of Anesthesia and Analgesia discussed three papers. Continuing the theme of neurotoxicity of inhaled anesthetics he posed the question, does anesthesia make you stupid?
He started by asking the audience two questions: Do you obtain separate anesthesia consent? The response was: Yes 65%, No 35%. The second question: Do you inform the patients/parents about neurotoxicity of inhaled anesthetics? Yes 13%, No 87%.
He presented the paper from the group at Columbia University in NYC, which was a retrospective review of 10,450 siblings from the NY State Medicaid database.
Early childhood exposure to anesthesia and risk of developmental and behavioral disorders in a sibling birth cohort. DiMaggio C, Sun LS, Li G. Anesth Analg. 2011; 113:1143-51
The clinical relevance of in vitro and in vivo studies showing neurotoxic effects of anesthetics on the developing brain remains unclear. Using data from a sibling birth cohort, they assessed the association between exposure to anesthesia in the setting of surgery in patients younger than 3 years and the risk of developmental and behavioral disorders. The exposed group was 304 children without a history of developmental or behavioral disorders who underwent surgery when they were younger than 3 years. The unexposed group was 10,146 children who did not receive any surgical procedures when they were younger than 3 years. The authors found that the estimated hazard ratio of developmental or behavioral disorders associated with any exposure to anesthesia when children were younger than 3 years was 1.6. The risk increased from 1.1 for 1 operation to 2.9 for 2 operations and 4.0 for ≥3 operations. When they looked at 138 sibling pairs where one sibling received anesthesia and one did not, the relative risk was 0.9 indicating no difference in developmental delay. Dr. Davis commented that on the surface the data seemed compatible with previous animal and human data, but a closer look raised more questions than answers.
2. Allergic reactions during anesthesia at a large United States referral center. Gurrieri C, Weingarten TN, Martin DP et al. Anesth Analg 2011; 113:1202-12
In this retrospective study, the Mayo Clinic Division of Allergic Diseases skin test database between 1992 to 2010 containing records of all patients who were tested for perioperative and anesthetic medications were reviewed to determine perioperative anaphylactic reactions. Thirty-eight patients were found to have an anaphylactic reaction during anesthesia, of which 18 were immunoglobulin (Ig)E-mediated anaphylactic reactions (likely causative agent identified by skin test), 6 were non-IgE-mediated anaphylactic reactions (elevated tryptase levels and negative skin test), and 14 were probable non-IgE-mediated anaphylactic reactions (tryptase levels normal or not obtained and negative skin test). Of the IgE-mediated reactions, antibiotics were the most likely causative agent (50%) whereas neuromuscular blocking drugs were implicated as a likely agent in 11% of reactions.
On the subject of allergic reactions to propofol in egg-allergic children, Dr Davis asked the audience: Do you give propofol to children with an egg allergy? The response was: Yes 67%, No 33%.
3. Allergic reactions to propofol in egg-allergic children. Murphy A, Campbell DE, Baines D, Mehr S. Anesth Analg 2011; 113:140-4
In order to determine whether children with an immunoglobulin (Ig)E-mediated egg and/or soy allergy had an allergic reaction after propofol use, a retrospective case review was performed of children with IgE-mediated egg and/or soy allergy who received propofol over an 11-year period (1999-2010). Twenty-eight egg-allergic patients with 43 propofol administrations were identified. No child with a soy allergy who had propofol was identified. Most children (68%) had a history of an IgE-mediated clinical reaction to egg with evidence of a significantly positive egg white skin prick test (SPT) reaction. There was one non-anaphylactic immediate allergic reaction that occurred 15 minutes after propofol administration in a 7-year-old boy with a history of egg anaphylaxis and multiple other IgE-mediated food allergies (cow's milk, nut, and sesame). SPT to propofol was positive at 3 mm. No other egg-allergic child reacted to propofol. Despite current Australian labeling warnings, propofol was frequently administered to egg-allergic children. Propofol is likely to be safe in the majority of egg-allergic children who do not have a history of egg anaphylaxis.
Last but not least, Dr. Charles Coté (Massachusetts General Hospital) presented a thorough review of the journal Pediatric Anesthesia which publishes only pediatric anesthesia topics as the name implies. He mentioned that eighty five papers, sixty seven review articles and eleven themed issues during the year were noteworthy. He went on to describe a number of “must read” papers, including:
- The severity and duration of postoperative pain and analgesia requirements in children after tonsillectomy, orchidopexy, or inguinal hernia repair. Stewart DW, Ragg PG, Sheppard S, Chalkiadis GA. Paediatr Anaesth. 2012; 22):136-43.
- Characterizing the behavior of children emerging with delirium from general anesthesia. Malarbi S, Stargatt R, Howard K, Davidson A. Paediatr Anaesth 2011; 21:942-50.
- Neurodevelopmental outcome following exposure to sedative and analgesic drugs for complex cardiac surgery in infancy. Guerra GG, Robertson CM, Alton GY, et al. Paediatr Anaesth 2011; 21:932-41
- Anesthesia and neurotoxicity to the developing brain: the clinical relevance. Davidson AJ. Paediatr Anaesth 2011; 21:716-21
- Should what we know about neurobehavioral development, complex congenital heart disease, and brain maturation affect the timing of corrective cardiac surgery? DiNardo JA. Paediatr Anaesth 2011; 21:781-6
- Cardiac arrest in anesthetized children: recent advances and challenges for the future. Morray JP. Paediatr Anaesth 2011; 21:722-9
- Probability of survival based on etiology of cardiopulmonary arrest in pediatric patients. Berens RJ, Cassidy LD, Matchey J, Campbell D, et al. Paediatr Anaesth 2011; 21:834-40
- Factors influencing blood loss and allogeneic blood transfusion practice in craniosynostosis surgery. Van Uitert A, Megens JH, Breugem CC, Stubenitsky BM, et al. Paediatr Anaesth 2011; 21:1192-7.
- Time-dependent perioperative anesthetic management and outcomes of the first 100 consecutive cases of spring-assisted surgery for sagittal craniosynostosis. Ririe DG, Smith TE, Wood BC, et al. Paediatr Anaesth 2011; 21:1015-9.
Dr. Coté also mentioned "quick hits" on preoperative fasting, ultrasound for stomach contents, dexmedetomidine and pain in PACU.
This was a very informative and interesting session in all with enthusiastic audience participation when questions were posed to the audience.
Is this SPA’s youngest abstract presenter?

Greg Hammer MD (Stanford University, Palo Alto) asks “Is Sara Connolly SPA’s youngest abstract presenter?”
Sara Connolly, a junior at Princeton University studying Ecology and Evolutionary Biology, plans to attend medical school following graduation from Princeton. Sara worked as a Research Assistant in my lab for the past two summers. She was working on an NICHD-funded study of the pharmacology of sodium nitroprusside.
As part of this work, Sara analyzed data from 60 children who received SNP for deliberate hypotension during major craniofacial and spinal fusion surgery. The incidence of metabolic acidosis in this population was compared to that in an age- and procedure-matched cohort of 119 patients from the same time period (2005-20). All children in the study were cared for at Lucile Packard Children's Hospital at Stanford.
The sample size in the control group was selected to achieve 80% power when testing non inferiority in the proportion of SNP patients with metabolic acidosis. Metabolic acidosis was defined as serum bicarbonate (HCO3) < 18.5 mEq/L and/or administration of HCO3 during anesthesia. The incidence of metabolic acidosis was similar in both groups (32% in the SNP group and 37% in the control group).
We concluded that SNP is not associated with metabolic acidosis during intraoperative infusion in children.
Personal Statement From a Resident
 By Kendra Buscetta
By Kendra Buscetta
CA3 resident
Department of Anesthesiology and Pain Medicine,
University of Washington School of Medicine
The alarm clock rang. It was much earlier than he normally woke up. He hit the snooze button hoping it was just a dream. His mother knocked on the door and slowly opened it. “Sweetie, it’s time to get up and get ready.” He dragged himself out of bed and slowly moped to the bathroom to brush his teeth. Today was the day he had been dreading for weeks. It seemed like it would never come, but here it was. It was raining. As he brushed his teeth, he tried to imagine what it would be like. Would it make him better? Would it hurt a lot? Would it make his mom stop crying at night after she thought everyone in the house was fast asleep? He spit out his toothpaste and told himself to be brave. When you are seven years old, you really aren’t certain what it means to be brave. But you know that you are scared and you can tell that you are not the only one.
He picked out his favorite stuffed bear from the shelf and jumped into the car. No breakfast this morning. He hugged his bear as his stomach grumbled. When they arrived at the hospital, his mother started filling out all of the paperwork. He sat on the seat with his bear, staring across the waiting room at all of the strangers. Were they all as scared as he was? He wanted to ask the others if they had been here before or if they knew what it was like, but he was shy. He had heard there were going to be really big needles and scary people in masks. He had been having nightmares about it all week.
Soon he met the nurse who greeted him with a big smile and gave his bear a tap on the head. The nurse was very kind and helped him to change into his hospital pajamas. Then another warm smiling face appeared at the door. She was wearing pajamas too and a funny hat with dinosaurs on it. She introduced herself as the doctor that would help him sleep through his surgery, and she sat down on the floor below his chair. The doctor asked questions about his bear and about school. She promised there wasn’t anything to worry about. She said that she had magical candy-flavored air and that all he would have to do is breathe it through a mask like astronauts do in space. Then he would get very sleepy and the next thing he knew he would be in the recovery room eating a popsicle and waiting to see his parents. What about the needles? The doctor said there wouldn’t be any needles until after he was asleep and he wouldn’t even know about them. The doctor said his mom could walk back to the operating room and stay until he was asleep and his bear could stay the whole time!
A huge relief washed over his face, and he sighed. The doctor noticed this and grinned. He stood up and took his mother’s hand tightly. They followed the doctor quietly down the hallway. After a few steps, he handed his bear to her mother and took the doctor’s hand as well. The doctor looked down at him and smiled. The three walked to the operating room hand in hand. He was grateful for the doctor’s reassurance and he was no longer scared. In those few precious minutes, he had come to trust her. What he did not know was that this moment was just as important to the doctor, who knew the second that boy took her hand that she was bound for a different path in life than she had expected. She knew that this feeling was priceless, and she would soon find it irreplaceable.
Eulogy for Dr. Mark I. Rossberg
By Myron Yaster, MD
Richard J. Traystman Professor of Pediatric Anesthesiology, Critical Care Medicine, and Pediatrics
The Johns Hopkins University
 Dr. Mark I. Rossberg, a pediatric anesthesiologist at the Johns Hopkins Children's Center and an assistant professor of anesthesiology and critical care medicine at the Johns Hopkins University School of Medicine, died at his Northwest Baltimore home of prostate cancer. He was 50. Mark was a superbly talented anesthesiologist and a beloved and masterful clinician-educator who trained a generation of anesthesiologists and pediatricians. A larger-than-life figure with a gregarious personality, Mark was a large burly man with a beard. He was an Orthodox Jew who was seldom without his yarmulke. Extremely cheerful, very caring, and a tireless worker, he was always the first one in and the last one out.
Dr. Mark I. Rossberg, a pediatric anesthesiologist at the Johns Hopkins Children's Center and an assistant professor of anesthesiology and critical care medicine at the Johns Hopkins University School of Medicine, died at his Northwest Baltimore home of prostate cancer. He was 50. Mark was a superbly talented anesthesiologist and a beloved and masterful clinician-educator who trained a generation of anesthesiologists and pediatricians. A larger-than-life figure with a gregarious personality, Mark was a large burly man with a beard. He was an Orthodox Jew who was seldom without his yarmulke. Extremely cheerful, very caring, and a tireless worker, he was always the first one in and the last one out.
Mark graduated in 1979 from the Bronx High School of Science and in 1987 from the combined seven-year BA-MD program at City College of New York and the Mount Sinai School of Medicine. After completing residencies in pediatrics and anesthesiology at Columbia Presbyterian Hospital, he went on to complete a fellowship in pediatric anesthesia and critical care medicine at the Children's Hospital of Philadelphia. He was recruited to Hopkins in the mid-1990s and quickly established himself as a person who had a superb talent for teaching residents and fellows.
Mark was considered by colleagues as a master of airway management and was often called upon to handle the most challenging and difficult cases. He had a phenomenal reputation. His colleagues would often request him for themselves or their families, not only because of his skill but because he employed his considerable charm and lightheartedness in calming nervous children and their families. Finally, Mark was “old school”. He understood that being a doctor was a privilege and because of that, patients always came first. As he often said, he was “doctor and not a health care provider”. He imparted his value system to his students and not surprisingly was voted by the anesthesiology house staff at Hopkins as Teacher of the Year. He is survived by his wife of 18 years, the former Esti Weissman; five children; his mother; and a sister.
He will be sorely missed and never forgotten.
Peds Passport
 By Helen V. Lauro, MD, MPH, FAAP
By Helen V. Lauro, MD, MPH, FAAP
NOTE:
Purchase of travel insurance with air evacuation coverage is highly recommended to meeting attendees and their families
2012
July 28-29: Chengdu, Sichuan Province, China
10th Asian Society of Paediatric Anaesthesiologists meeting
Tel: +8613982269741 or +8618980601541, Fax: +862885423593
Information: Dr. Jing Lin or Dr. Yunxia Zuo, Dept. of Anesthesiology, West China hospital, Sichuan University, Chengdu, China
Website: http://www.aspa-2000.com/meetings.html
Email: ruan_lin820@hotmail.com or zuoyunxia666@gmail.comAugust 26: Milan, Italy
“The Basic and Clinical Science of Challenging Pediatric Pain Syndromes," official satellite symposium of the 14th World Congress on Pain
Tel: +41 22 33 99 593, Fax: +41 22 33 99 631
Information: MCI Suisse on behalf of IASP, 75 Rue de Lyon, CH – 1211 Geneva 13 – Switzerland
Website: http://www.iasp-pain.org/AM/Template.cfm?Section=Childhood&Template=/CM/HTMLDisplay.cfm&ContentID=8433Email: iasp2012@mci-group.comSeptember 6-9: Santa Monica, California, USA
19th Pediatric Critical Care Colloquium
Tel: (323)-361-7105; Fax: (323)-361-1001
Information: Ms. Ginger Mallas, Practice Manager, Children’s Hospital Los Angeles, Dept. of Anesthesiology, 4650 Sunset Blvd. Mailstop #3, Los Angeles, CA 90027
Website: http://www.pcccolloquium.com
Email: gmallas@chla.usc.eduSeptember 7-10: San Francisco, California, USA
Pediatric Sedation Outside the Operating Room
Tel: (617)-355-5775; Fax: (617)-730-0610
Information: Amanda Buckley, Children’s Hospital Boston, Department of Anesthesia, 300 Longwood Avenue, Boston, Massachusetts 02115
Website: http://www.pediatricsedationconference.com
Email: amanda.buckley@childrens.harvard.eduSeptember 20-22: Stresa, Italy
Annual Congress of the European Society for Paediatric Anesthesiology: Stresa 2012
Tel: +31 (0) 887555555; Fax: +31 (0) 887554702
Information: Secretariat ESPA, c/o Department of Anesthesia, Intensive Care and Emergency Medicine, Wilhelmina Children Hospital/University Medical centre Utrecht Lundlaan 6, Mail stop: KG 02.307.1, PoBox 85090, 3508 AB Utrecht, The Netherlands
Website: http://www.euroespa.org
Email:secretary@euroespa.orgSeptember 24-27: Boston, Massachusetts, USA
6th Annual Pediatric Anesthesia Review (Jointly sponsored by Baylor Health Care System and A. Webb Roberts Center for Continuing Medical Education)
Tel: (800)-222-6927
Information: Northwest American Seminars, P.O. Box 2797, Pasco, WA 99302
Website: http://www.nwas.com
Email: info@nwas.comSeptember 29: Boston, Massachusetts, USA
The Art & Science of Pediatric Pain and Management 2012
Tel: (617)-355-7155; Fax: (617)-384-8686
Information: Boston Children’s Hospital, Nursing Staff Development, Nursing Office, Wolbach 201, 300 Longwood Avenue, Boston, MA 02115
Website: http://cme.hms.harvard.edu/index.asp?SECTION=CLASSES&ID=03214516&SO=NEmail: staffdevelopment@childrensharvard.eduOctober 5-9: Istanbul, Turkey
4th Congress of the European Academy of Paediatric Societies/23rd European Society of Paediatric and Neonatal Intensive Care (ESPNIC) Medical and Nursing Congress
Tel: + 41 22 908 0488 Fax: + 41 22 906 9140
Information: ESPNIC Administrative Office, c/o Kenes International, 1-3 Rue de Chantepoulet, P.O. Box 1726, CH-1211, Geneva 1, Switzerland
Website: http://www.espnic.de
Email: reg_eaps12@kenes.comOctober 11-12: Washington, D.C., USA
International Assembly for Pediatric Anesthesia Safety Knows No Borders
Tel: (804)-282-9780, Fax (804)-282-0900
Information: Society for Pediatric Anesthesia, 2209 Dickens Road, Richmond, VA 23230-2005
Website: http://www.internationalassembly2012.org
Email: spa@societyhq.comNovember 16-18: San Antonio, Texas, USA
2012 Pediatric Anesthesia Conference: New Frontiers in Pediatric Anesthesia
Tel: (682)-885-3841, 682-885-4054
Information: Ms. Amanda Mrstik, Cook Children’s Hospital, Cook Children's Anesthesiology Services
801 Seventh Avenue, Fort Worth, TX 76104
Website: https://secure.cookchildrens.org/Education/UserPortal/Course.aspx?CourseID=300
Email: Amanda.mrstik@cookchildrens.orgNovember 22-25: Melbourne, Victoria, Australia
Society for Paediatric Anaesthesia in New Zealand and Australia (SPANZA) Conference 2012:
Spring Into the Future New Directions in Paediatric Anaesthesia
Tel: +61 2 4973 6573, Fax: +61 2 4973 6609
Information: SPANZA Secretariat, P.O. Box 180, Morriset, New South Wales, Australia 2264
Website: http://www.willorganise.com.au/spanza2012/
Email: spanzaconf@willorganise.com.au2013
February 17-22: Capetown, South Africa
6th World Congress of Paediatric Cardiology & Cardiac Surgery
Tel: +27 21 532 6333, Fax: +27 21 532 6331
Information: PCCS Conference Secretariat, Global Conferences, P.O. Box 632, Howard Place, Pinelands 7450
Website: http://www.pccs2013.co.za
Email: info@pccs2013.co.zaMarch 14-17: Las Vegas, Nevada, USA
Society for Pediatric Anesthesia (SPA)/American Association of Pediatrics (AAP) 2013 Winter Meeting
Tel: (804)-282-9780, Fax (804)-282-0900
Information: Society for Pediatric Anesthesia, 2209 Dickens Road, Richmond, VA 23230-2005
Website: http://www.pedsanesthesia.org
Email: spa@societyhq.comMay 31-June 2: Aurora, Colorado, USA
VII International Symposium on the Pediatric Airway (ISPA)
Tel: (720)-848-6710; Fax: (720)-848-7375
Information: Ms. Beverly Janik, Project Coordinator, Dept. of Anesthesiology, University of Colorado Denver, B113, Leprino Bldg, 7th Floor, 12401 East 17th Avenue, Aurora, CO 80045
Website: http://www.pedsairwaysymposium.org
Email: Beverly.janik@ucdenver.eduJune 17-20: Stockholm, Sweden
Ninth International Symposium on Pediatric Pain 2013
Tel: +46 8 5465 1500
Information: Congress Secretariat, MCI Stockholm Office, P. O. Box 6911, SE-102 39 Stockholm
Website: http://www.ispp2013.org, http://www.mci-group.com/sweden
Email: confirmation-sweden@mci-group.com
June 20-21: Cambridge, United Kingdom
Association of Paediatric Anaesthetists of Great Britain and Ireland (APAGBI) Joint Meeting with European Society for Paediatric Anesthesiology (ESPA)
Tel: +44 (0) 20 7631 8887, Fax: +44 (0) 20 76314352
Information: APA Administration Office, AAGBI, 21 Portland Place, London, W1B 1YP, United Kingdom
Website: http://www.apagbi.org.uk
Email: apagviadministration@aagbi.orgSeptember 5-7: Geneva, Switzerland
Annual Congress of the European Society for Paediatric Anaesthesioloogy: Geneva 2013
Tel: +31 (0) 887555555; Fax: +31 (0) 887554702
Information: Secretariat ESPA, c/o Department of Anesthesia, Intensive Care and Emergency Medicine, Wilhelmina Children Hospital/University Medical centre Utrecht Lundlaan 6, Mail stop: KG 02.307.1, PoBox 85090, 3508 AB Utrecht, The Netherlands
Website: http://www.euroespa.org
Email: secretary [et[ euroespa.orgOctober 11: San Francisco, California, USA
Society for Pediatric Anesthesia (SPA) 27th Annual Meeting
Tel: (804)-282-9780, Fax (804)-282-0900
Information: Society for Pediatric Anesthesia, 2209 Dickens Road, Richmond, VA 23230-2005
Website: http://www.pedsanesthesia.org
Email: spa@societyhq.com2014
March 6-9: Fort Lauderdale, Florida, USA
Society for Pediatric Anesthesia (SPA)/American Association of Pediatrics (AAP) 2014/Congenital
Cardiac Anesthesia Society (CCAS) Winter Meeting
Tel: (804)-282-9780, Fax (804)-282-0900
Information: Society of Pediatric Anesthesia, 2209 Dickens Road, Richmond, VA 23230-2005
Website: http://www.pedsanesthesia.orgMay 15-16: Leeds, United Kingdom
Association of Paediatric Anaesthetists of Great Britain and Ireland Meeting
Tel: +44 (0) 20 7631 8887, Fax: +44 (0) 20 76314352
Information: APA Administration Office, AAGBI, 21 Portland Place, London, W1B 1YP, United Kingdom
Website: http://www.apagbi.org.uk
Email: apagviadministration@aagbi.org
Please forward all information concerning congresses relevant to Pediatric Anesthesia to:
Helen V. Lauro, MD, MPH, FAAP, SUNY Downstate Medical Center University Hospital of Brooklyn at Long Island College Hospital, Department of Anesthesiology, 339 Hicks Street, Brooklyn, New York 11201.