SPA Annual Meeting Reviews
Session I: Mechanisms of Consciousness
By Jerry H. Kim, MD
Seattle Children’s Hospital
Monitoring the Pediatric Brain under General Anesthesia
The first lecture was given by Emery N. Brown, MD, PhD (Massachusetts General Hospital), who kicked off the annual Myron Yaster, err… SPA Annual Meeting with a lecture on monitoring the pediatric brain under general anesthesia. Dr. Brown started first by saying that it was a great time to be a pediatric anesthesiologist! (More on that later). He then provided the overview of his talk: first, a discussion of what is known about the way different stages of general anesthesia looks in adults (focusing on how EEG signatures correspond with neural circuits), before concluding with what general anesthesia looks like in children, as a function of age.
Dr. Emery Brown
Monitoring changes in consciousness yields rich data. He illustrated this point by showing a video of the EEG of a 65 year old woman receiving propofol during induction for a thyroidectomy. As the propofol was first injected, the EMG signal increased, likely in response to the pain commonly felt on injection. This was followed by beta waves at 13Hz, then slow oscillations and large amplitude oscillations. Next came burst suppression, and finally an isoelectric line.
EEG data is particularly rich since it changes quickly over time and has ~ 100:1 signal to noise ratio, in contrast to the relatively static and noisy fMRI data. There are also many ways to visualize the data, including the traditional EEG trace over time in two dimensions, or a more complex spectral analysis, which can graph power and frequency vs. time in three dimensions. The latter can be reduced to two dimensions by graphing frequency vs. time, meanwhile preserving data by indicating the power as a color heat-map.
Further dimensions can be added by including the location of the recording within the three-dimensional structure of the brain. Dr. Brown explained this more eloquently than I could, and compressed this highly dimensional data into a series of slides that were easy to digest. On one slide, he displayed several dozen graphs positioned along concentric circles which represented the electrode’s position on the scalp, preserving anterior/posterior and left/right relationships. He then animated the slide, showing how the signals changed over time. As you can tell, this is very difficult to explain in words, but a static image of this slide is included below which may help:
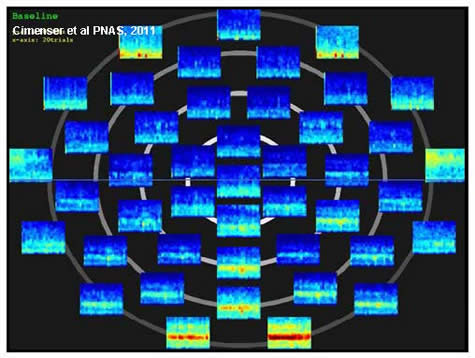
He displayed this useful visualization to present the results from a very interesting study he co-authored. In it, adults were asked straightforward yes or no questions. For example, a tone was played and the participant was asked, “Is this a high tone?” Or they were shown a word and asked, “Is this your name?” Propofol was then infused until they lost ability to answer questions about words, and then about the sounds. As it turns out, there is a temporal and spatial dynamic to the frequency changes which appear during the different stages of consciousness. Occipital alpha oscillations at 10Hz, present when the eyes are closed, move from the back of the head to the front (anteriorization). Present in about 90% of people, these oscillations get a little weaker as we age. Dr. Brown also said this 10Hz signal was “highly coherent,” which I assume to mean that it is better off than I am after finishing one of New Orleans’ signature drinks, the Hurricane. Actually, I believe coherence in the science of signal processing is a measure of the similarity between multiple signals or datasets.
To summarize the EEG changes during propofol-induced loss of consciousness, there are four notable changes: alpha oscillations at 8-12Hz, fragmentation of the cortex marked by slow oscillations (<1Hz), anteriorization of oscillation caused by frontoparietal disconnect, and inactivation of arousal centers in the brainstem. Disruption of coupling between the thalamus and cortex appears to be the cause of both the alpha and slow oscillations.
In the thrilling conclusion of Dr. Brown’s talk, he discussed the findings of anesthetic-induced loss of consciousness as a function of age. There is good evidence that EEG changes are age-dependent, which he demonstrated by showing spectrograms from a three year-old, a 14 year-old and 30 year-old. Although the spectrograms presented were on different time scales, it appeared that the younger patients’ spectrograms showed higher power in the 0-5 Hz range and the 10-20 Hz range. However, Dr. Brown also pointed out that the differences are also highly variable from individual to individual. As evidence, he also showed the spectrograms of a 56, 57, and 81 year-olds. The 57 year-old looked similar to the 30 year-old, while the 56 year old looked most similar to the 81 year-old. Overall amplitude peaks at 4-5 years of age, but declines with age thereafter. In contrast, coherence is weak before 4-5 years of age, but remains strong across all ages greater than 4-5 years. In collaboration with Charles B. Berde, MD, PhD, Dr. Brown and Dr. Berde have found that alpha oscillations appear at 3-4 months of age, increasing markedly in amplitude by 4-6 months. In results consistent with others, they also found no coherent activity in any 0-6 month old, and coherence does not appear meaningfully strong until 14-15 months of age.
Dr. Brown concluded his talk with a few important summary statements. He reiterated that anesthetics create altered arousal states by changing brain dynamics, the nature of which change with age likely in relation to brain development. He is hopeful and excited about future scientific advances in this field, which brings us back to why he is so excited about pediatric anesthesiology as a field right now. He believes that understanding these changes in dynamics will allow us to understand anesthetic mechanisms more precisely, to develop better methods for monitoring the anesthetized brain (especially for children), and to develop new approaches for creating states of general anesthesia and sedation.
Next, George A. Mashour, MD, PhD (University of Michigan Medical School), presented his lecture on consciousness and anesthesia. He started by disclosing a pending patent he owns “on the use of directional/effective connectivity for measuring states of consciousness.” He then dove right in with a statement he described as somewhat controversial, but one he believed in: spatio-temporal integration of neural information is necessary for consciousness. It appears he lead with this statement because it likely fundamentally shapes the way he views consciousness and wakefulness.

Dr. George Mashour
Next came definitions of terms used throughout the talk, which I have stated here for clarity. He described wakefulness as the manifestation of being awake in a sleep/wake in the absence of (or perhaps without regard to) experience. In contrast, awareness refers to the experiential component of consciousness. These two states can be thought of as being on a spectrum, with general anesthesia, coma, sleep, locked-in syndrome, and vegetative state also on this spectrum.
He then delved deeper into descriptors of consciousness: levels vs. contents, phenomenal vs. access, and connected vs. disconnected. Levels of consciousness refer to the “state,” while contents refer to the particular qualities (or qualia) of consciousness. Phenomenal consciousness is pure experience, while access refers to the availability of the experience. Connected consciousness relates to environmental stimuli, while disconnected consciousness relates to endogenous experience. Finally, he described easy problems of consciousness as those that related to integration, verbal report, etc, whereas hard problems refer to those related to the experience itself. He stressed that current knowledge does not explain the experiential component of consciousness.
With those out of the way, he moved onto the neurobiology of consciousness and general anesthesia. As one passes from wakefulness to non-REM to REM sleep, each state is characterized by the activation of different receptors in different regions of the brain. There is also evidence that experience is different from consciousness, in that consciousness is not correlated with primary sensory processing. He showed a fascinating series of fMRI images of the brains of children at different ages: newborn, one year-old, and two years old. Excitingly, your intrepid reviewer could easily appreciate the increased connectivity between brain regions in the older children. The difference is most marked between the newborn brain vs. the one and two year-old brains. By extension into the fetal period, consciousness is likely impossible without the development of thalamocortical connections, which occur at or after 24 weeks of gestation.
Subliminal processing of information also appears distinct from conscious processing. Whereas the occipital cortex appears to dominate in response to subliminal stimuli, conscious processing peaks in prefrontal areas. Furthermore, incomplete myelination in younger children appears to cause slower transmission of electrical impulses between the brain regions required for conscious processing.
Transitioning to the effects of anesthetics on conscious processing, Dr. Mashour next posited that anesthetic-induced unconsciousness is also not correlated with primary sensory processing. During both anesthesia and sleep, the frontoparietal networks are deactivated. One study found that at low isoflurane levels, long-latency potentials are suppressed in humans, specifically those that travel from frontal to occipital cortex. At higher levels of isoflurane, both directions are suppressed. In rats, there also appears to be selective inhibition of feedback connectivity during anesthesia, particularly in the frontoparietal and frontooccipital direction.
Frontoparietal suppression and disruption is also the hallmark of unconsciousness during propofol administration. Dr. Mashour expanded on anesthetic-specific network fragmentation (using slides which I do not believe made it into the PDF of his lecture slides available for download.) Here, he proposed that propofol reduces the capacity for integration, and sevoflurane result in disrupted phase relationships. He believes the thalamocortical system also plays a role in anesthetic-induced unconsciousness.
Finally, he discussed ketamine, which is different than most other anesthetics in that it generally increases EEG activity after administration rather than decreasing or slowing. However, ketamine depresses the thalamus and disrupts frontoparietal phase relationships as well. In conclusion, he stated that network disruption appears to be a characteristic shared across multiple anesthetic drug classes.