OS1-132
Older age attenuates excess risk associated with congenital heart disease in pediatric non-cardiac surgery
Miller R, Tumin D, Tobias J, McKee C
Nationwide Children's Hospital, Columbus, OH, US
Background: As management of congenital heart disease (CHD) improves, children with CHD increasingly present for non-cardiac surgery. Prior studies report conflicting results on the association between CHD and adverse outcomes in non-cardiac surgery. Although some studies have found an increased risk associated with CHD when examining non-cardiac procedures, analyses of procedures that primarily involve older children and adolescents have reported no such association. We evaluated whether the association between CHD and children’s adverse surgical outcomes was attenuated by older age.
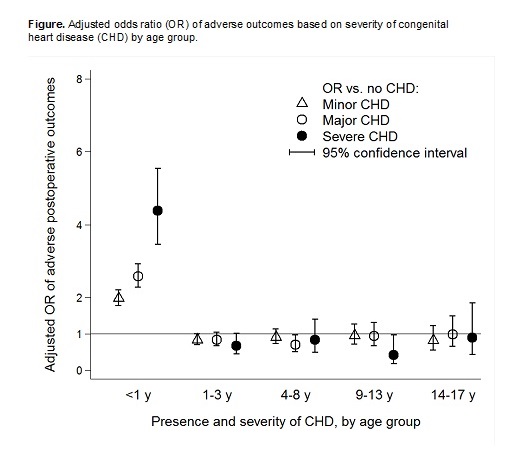
Methods: Patients 0-17 years of age undergoing elective non-cardiac surgery were identified in the National Surgical Quality Improvement Program-Pediatric registry. CHD status was classified as none, minor, major, or severe. Multivariable logistic regression evaluated the association between CHD status and any postoperative complications for groups defined by patient age (<1, 1-3, 4-8, 9-13, and 14-17 years). Complications included cardiac arrest, reintubation, infection, renal failure, neurological complication, thromboembolic complication, reoperation, 30 day unplanned revisit, 30 day prolonged hospital stay, and mortality.
Results: The analysis included 131,164 children, of whom 6,420 had minor CHD, 3,825 had major CHD, and 963 had severe CHD. The overall rate of complications was 9%. In multivariable analysis, children <1 years old had greater risk of postoperative complications if they had minor (OR=2.0; 95% CI: 1.7, 2.2; p<0.001), major (OR=2.6; 95% CI: 2.3, 2.9; p<0.001), or severe CHD (OR=4.4; 95% CI: 3. 5, 5.5; p<0.001). In older age groups, however, the presence of CHD was not independently associated with postoperative complications (Figure).
Discussion: In elective non-cardiac pediatric surgery, excess risk of postoperative complications attributable to CHD was only evident among infants and not older children. This finding reconciles results from prior analyses of NSQIP that focused on cohorts of older children (e.g., children undergoing posterior spinal fusion), where CHD lacked an independent association with adverse outcomes. Among older children, recognition of specific risk factors apart from CHD (including risk factors influenced by history of CHD) may be more relevant for risk adjustment. Alternately, mortality selection or improved management of CHD symptoms at older ages may contribute to equivalency of outcomes of non-cardiac surgery between older children with and without CHD.
References:
1. Faraoni D, Zurakowski D, Vo D, et al. Post-operative outcomes in children with and without congenital heart disease undergoing noncardiac surgery. J Am Coll Cardiol 2016;67:793-801.
2. Basques BA, Chung SH, Lukasiewicz AM, et al. Predicting Short-term Morbidity in Patients Undergoing Posterior Spinal Fusion for Neuromuscular Scoliosis. Spine. 2015;40:1910-7.
Top