NM-272
Unmet Need for Care Coordination among Children with Special Health Care Needs
Miller R, Tumin D, Hayes D, Uffman J, Raman V, Tobias J
Nationwide Children's Hospital, Columbus, OH, United states
Background: Coordination of children’s health care in a “medical home†has been endorsed by medical societies, health care institutions, and policy groups. Yet, previous studies have described socioeconomic disparities in children’s access to care coordination, especially among children with special health care needs (CSHCN). As policy incentives and technological innovation have supported dissemination of the medical home model, we used a recent nationally-representative survey to investigate whether child and family socioeconomic characteristics remain associated with unmet need for care coordination.
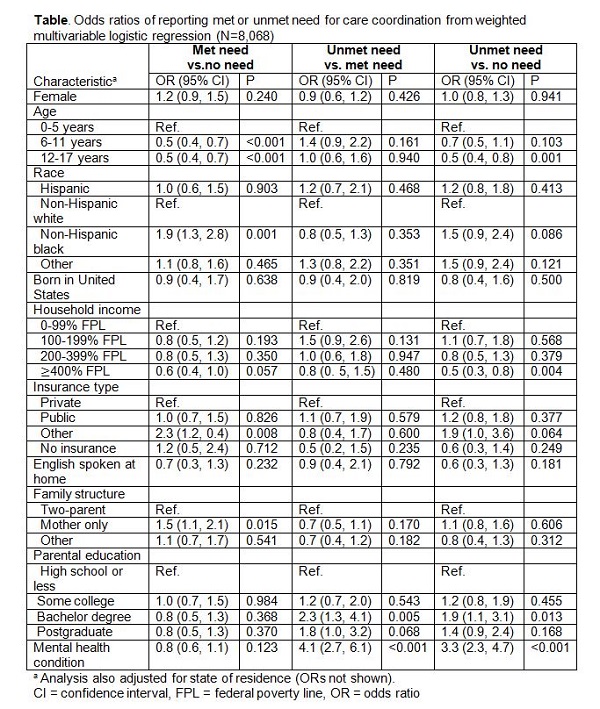
Methods: CSHCN (0-17 years of age) were identified in the 2016 National Survey of Children’s Health, according to screening questions about whether a child has a chronic medical condition and requires additional care, as compared to most children. CSHCN using ≥2 types of health services in the past year were selected for analysis, and care coordination was defined as help with arranging the child’s care among different doctors or services. Children were classified as (1) not needing care coordination, (2) receiving sufficient care coordination (met need), or (3) needing but not receiving care coordination (unmet need). Weighted multinomial logistic regression examined the odds of each outcome according to child and family characteristics.
Results: The analysis included 5,622 children with no need for care coordination, 1,466 with a met need, and 980 with unmet needs. Children with mental health conditions were more likely to have unmet rather than met needs for care coordination (OR=4.1; 95% CI: 2.7, 6.1; p<0.001). However, in multivariable analysis (Table), none of the socioeconomic characteristics (race/ethnicity, income, family structure, insurance coverage, place of birth, and use of English in the home) were associated with greater odds of unmet rather than met need for care coordination.
Discussion: In a recent survey, many caregivers of CSHCN still report unmet needs for care coordination. However, our study found none of the previously documented socioeconomic disparities in access to care coordination among children who need it. This suggests that remaining barriers to broader implementation of care coordination are related to institutional constraints rather than individual socioeconomic factors. Overcoming institutional barriers may require the allocation of funds and personnel to care coordination initiatives, as well as leveraging technology to improve communication and coordination across services.
References:
1. Toomey SL, Chien AT, Elliott MN, et al. Disparities in unmet need for care coordination: the national survey of children’s health. Pediatrics. 2013; 131:217-24.
2. Ferrari LR, Antonelli RC, Bader E. Beyond the preoperative clinic: Considerations for pediatric care redesign aligning the patient/family-centered medical home and the perioperative surgical home. Anesth Analg. 2015; 120:1167-70.
Top