PR1-156
A high baseline psycho-somatic symptom profile predicts persistent pain at one year following spine fusion in children.
Virani S, Malviya S, Tait A, Caird M, Farley F, Li Y, Weber M, Voepel-Lewis T
University of Michigan Health System, Ann Arbor, Michigan, United stated of america
BACKGROUND
A high preoperative symptom profile was recently associated with worse pain outcomes after posterior spine fusion (PSF).¹ This symptom profile was present in 30% of children and was differentiated by higher depression, fatigue, pain interference, neuropathic pain and pain catastrophizing characteristics. No studies have yet described whether such a pain vulnerable profile, similar to that in children with chronic or centralized pain, predicts long-term outcomes after PSF. This longitudinal study differentiated preoperative symptom profiles in children and examined whether a high symptom profile predicts ongoing pain and analgesic use 1 year after PSF.
METHODS
With IRB approval, written parental consent and child assent, children aged 10-17 years were surveyed before surgery and at 1 year after PSF. Baseline self-reported measures included pain intensity (0-10 numeric scale), pain location (body map), neuropathic pain (painDETECT), catastrophizing, fatigue, depression, anxiety, and pain interference (PROMIS short forms). Perioperative and postoperative analgesics were recorded. Children were re-surveyed at 1 year regarding pain intensity, pain interference, and analgesic use.
RESULTS
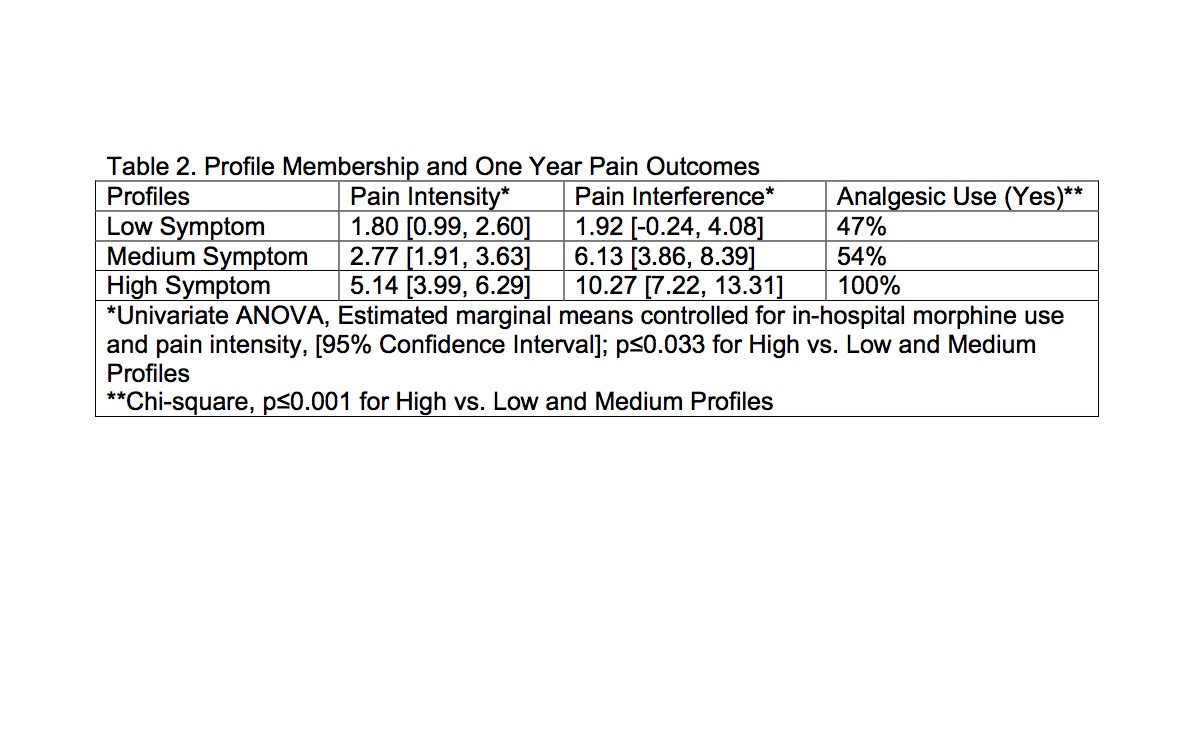
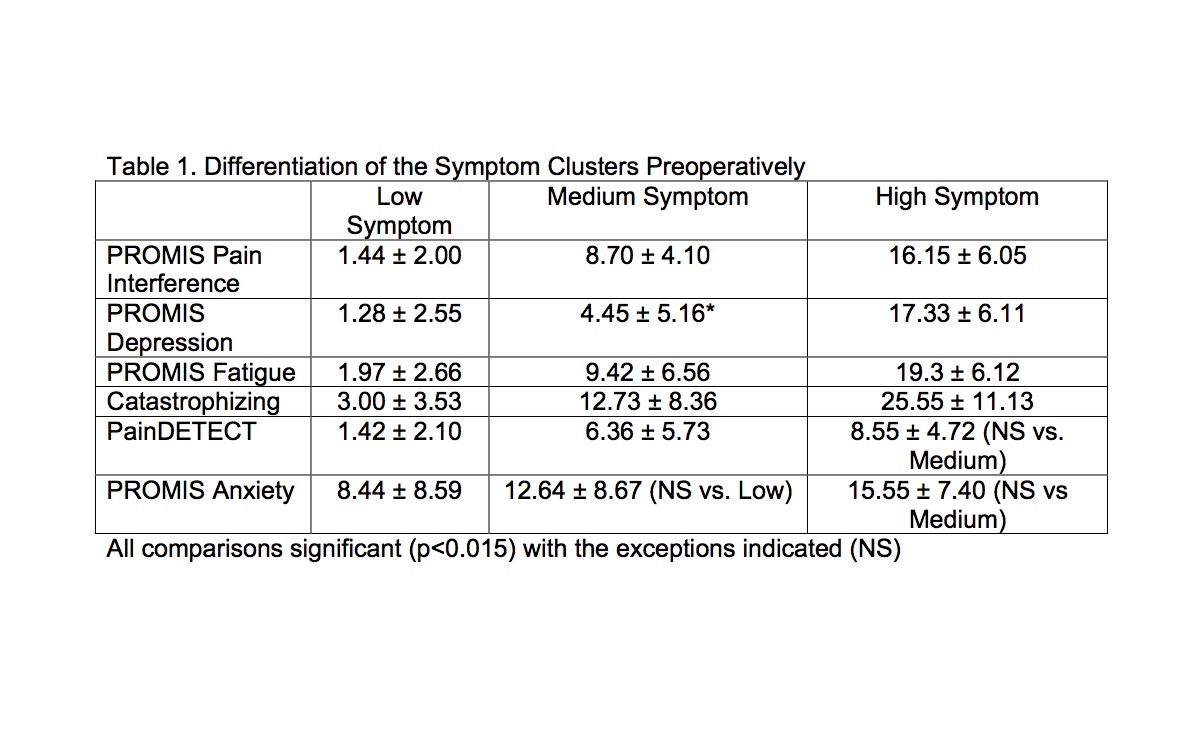
95 healthy children (75% female, 94% ASA 1-2) completed the study. A cluster analysis identified three symptom profiles at baseline, differentiated by pain interference, depression, fatigue, pain catastrophizing scores, and to a lesser extent by painDETECT and anxiety (Table 1). The number of painful body sites significantly correlated with symptom profile (rho=0.347, p<0.01). Compared to the low-medium symptom groups combined, the high symptom profile group included more girls (95% vs. 68%, p=0.019) but was not different in the involved spinal segments (70% vs 78% thoracolumbar), mode of perioperative analgesia (75% vs. 71% intrathecal morphine) or hospital opioid use (0.013 vs. 0.011 mEq/kg/hr, p=0.66). The high profile group reported more pain interference (10.13 vs. 3.95, p=0.003) and were more likely to be taking analgesics at 1 year (100% vs. 50%, p<0.001) compared to the low-medium symptom group. Controlled for hospital morphine consumption and pain scores, cluster membership predicted pain intensity and interference at 1 year (Table 2).
CONCLUSION
Findings show that children with higher psycho-somatic symptoms preoperatively may be at risk for persistent pain and analgesic use 1 year after surgery. Identifying such symptomology prior to surgery may help to strategize early interventions that could mitigate persistent postoperative pain after PSF.
REFERENCE
1. Voepel-Lewis T et al. Anesth Analg 2017;124:1594-602
Top