NM-204
SAFETY STOP: A valuable addition to the Pediatric Universal Protocol
Munshey F, Caruso T, Darling C, Tweedy M, Aldorfer B, Sharek P
Lucille Packard Children's Hospital Stanford, Stanford, CA, United states
Introduction
The World Health Organization (WHO) surgical checklist identifies three key times of a patient’ progression during a surgical encounter to minimize chances of error: the sign in, timeout, and sign out. As part of the “Safe Surgery Saves Lives†campaign, the WHO guidelines state that a timeout must be performed just prior to incision, after preparation and draping (P&D) of the patient to minimize surgical morbidity and mortality.
At our institution, prior to a routine visit by the Joint Commission (JC), a mock JC survey recorded that we performed timeouts prior to P&D of the patient, not afterwards as recommended by the WHO. This prompted a multidisciplinary effort aimed at reducing our regulatory risk and optimizing patient care. The goal of this study was to align our practice policy with regulatory requirements within four weeks.
Methods
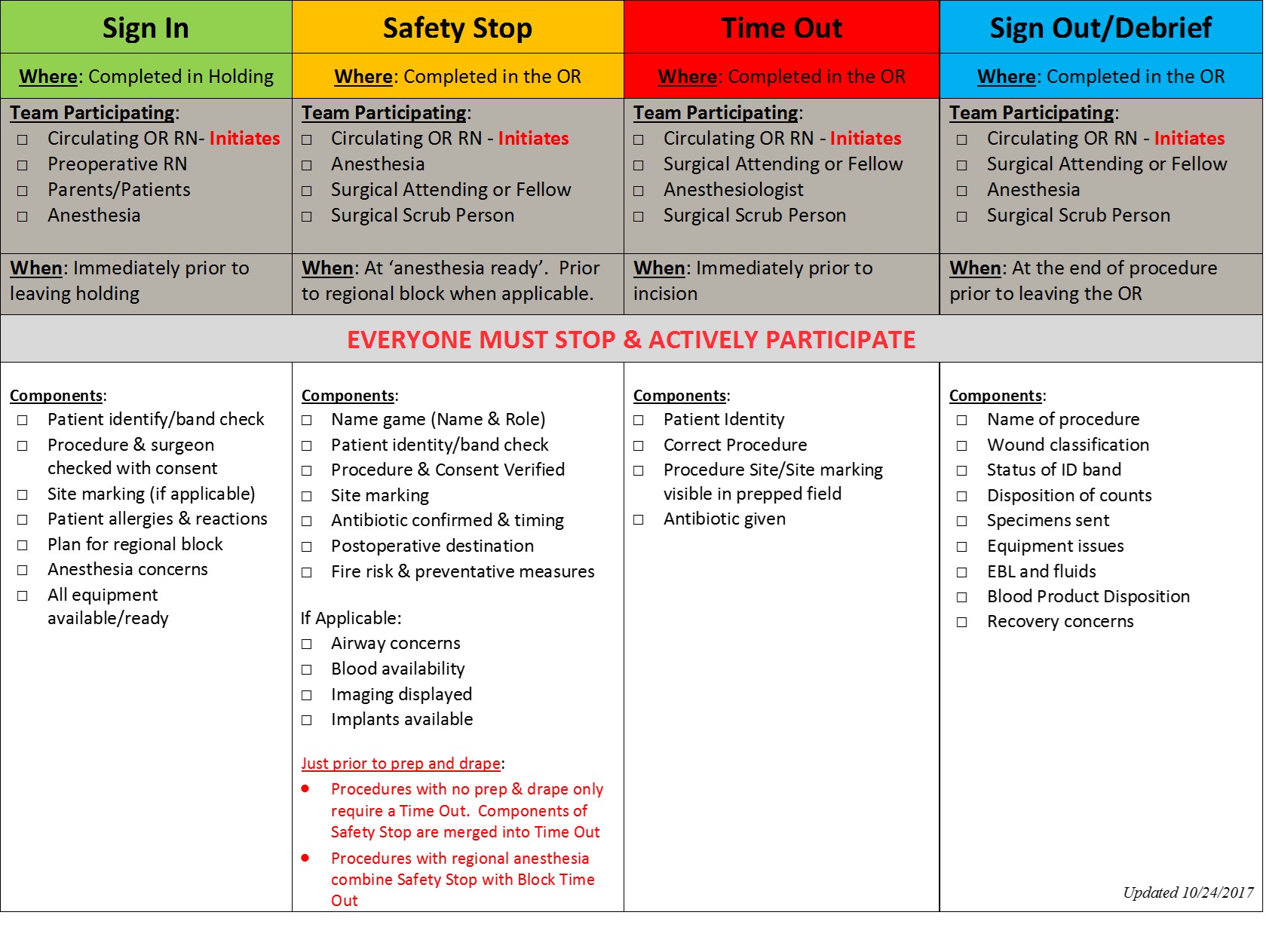
Beginning March 2016, the perioperative quality improvement (QI) team consisting of physicians, nurses, pharmacists, and quality managers utilized an A3 project plan to guide development of countermeasures. Current state analysis revealed that we intentionally performed timeouts prior to P&D to ensure the correct surgical site and patient were prepared. Unlike adults, the operative field of a pediatric patient can be quite small, increasing the possibility of wrong site preparation. Moving the timeout to after P&D presented too high a risk of increasing patient harm. After an analysis of the problem, we decided to implement a new component to the universal protocol, called the Safety Stop. The Safety Stop would occur just prior to P&D of the patient and the timeout would be performed just prior to incision, aligning with WHO recommendations. After electronic correspondence and several perioperative leadership meetings, the enhanced universal protocol was initiated. Compliance audits were performed by operating room nurses.
Results
By conscientiously gathering feedback from front line staff, we successfully initiated an optimized universal protocol, designed for pediatric patients. 60 audits were completed. Of those completed, 96% demonstrated compliance with the new policy. During the Joint Commission visit, our enhanced universal protocol with inclusion of the Safety Stop was highlighted as an area exceeding traditional standards.
Discussion
QI methodology was utilized to optimize the universal protocol for pediatric patients at our institution. Although initially we believed that simply moving the timeout from prior to P&D to just prior to incision would be a solution, further analysis revealed surgical concerns that were not apparent at first. Although there have been many reports of the effectiveness of the universal protocol, the authors are unaware of any specific to pediatric patients aiming to counter the potential risks associated with P&D small bodies and surgical sites.
Conclusion
A pediatric universal protocol was successfully implemented and well received by the JC.
Top