NM-366
Identification of preoperative intravascular epidural catheters with epidurograms in a patient undergoing bilateral Wilms' tumor resection
Starker E, Johnson B, Ing R, Ciarallo C, Iacovetto M, Merritt G
Children's Hospital of Colorado, Aurora, CO, USA
Epidural catheter placement for post-operative analgesia is a common technique used in children. Catheters can become non-functional due to failure to place or maintain the catheter in the epidural space. Epidurograms aid in the guidance of safe and efficacious epidural placement and the identification of misplaced catheters (1). Epidurograms add additional risk to the procedure, including increased cost, radiation exposure, or reactions to contrast dye (1). These risks must be weighed against the increased benefit of accurately identifying appropriately placed catheters, especially in a high-risk pediatric population.
Wilms’ tumor is the most common primary renal malignancy in children. Many patients require chemotherapy or other treatment modalities to shrink the tumor prior to resection due to the large size at presentation.
We describe the anesthetic management of an 18 month old female undergoing bilateral Wilms’ tumor resection complicated by two intravascular epidural placements preoperatively, followed by successful catheter placement postoperatively utilizing epidurogram guidance.
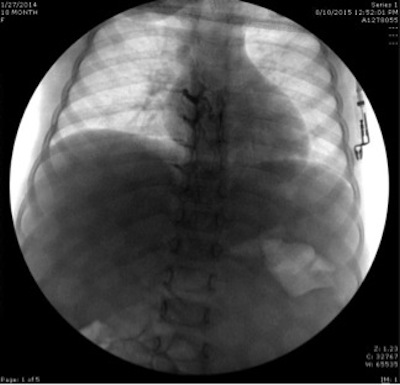
General anesthesia was induced and a thoracic epidural was placed in the T9-T10 interspace to loss of resistance technique to saline with the patient in left lateral positioning. Aspiration of the catheter was negative. An epidurogram was performed which demonstrated contrast material in the venous plexus of the T4-T8 region (see Figure 1). The catheter was removed and replaced with the same technique two levels inferiorly. Aspiration of the catheter and a test dose was negative. An epidurogram demonstrated contrast in T8-T9 region, with a possible vascular course. On repeat aspiration, blood was noted in the catheter, leading to catheter removal. After tumor resection and abdominal closure, a third epidural catheter was placed at T12-L1. An epidurogram demonstrated no vascular uptake of contrast and test dose was negative. An epidural infusion was initiated and the patient’s pain was well controlled postoperatively.
Epidurograms are a valuable method to verify epidural placement, especially in patients with intra-abdominal tumors. Patients with large abdominal masses have increased abdominal pressure, leading to epidural venous engorgement. It is important to recognize the epidural plexus enlargement in these patients and the resulting difficulty in epidural placement. The decreased abdominal pressure after tumor resection may have led to decreased distension of the epidural venous plexus, allowing for successful placement postoperatively. This case highlights the difficulty with preoperative epidural catheter placement in patients with large intra-abdominal tumors and the importance of epidurograms as a confirmation technique to ensure identification of misplaced catheters.
1. Taenzer, A. et al. Experience with 724 epidurograms for epidural catheter placement in pediatric anesthesia. Reg Anesth Pain Med. 2010; 35(5): 432-5.
Top