NM-207
Anesthetic Management of Congenital Central Hypoventilation Syndrome Patients
1Zhu J, 1Karnwal A, 2Chang G, 1Shin C, 1Keens T, 1Perez I
1Children's Hospital Los Angeles, Los Angeles, CA, USA; 2University of Southern California, Los Angeles, CA, USA
Introduction: Congenital Central Hypoventilation Syndrome (CCHS) is a rare neuropathological condition characterized by failure of the autonomic control of breathing during sleep. This has profound concerns for the anesthesiologist in the perioperative period due to absent ventilatory response to hypoxemia and hypercarbia [1]. As a referral center for CCHS, this study was done with an aim to evaluate our anesthetic practice and perioperative outcome among these patients at Children’s Hospital Los Angeles.
Methods: This IRB approved retrospective study included all CCHS patients who underwent procedures under general anesthesia (GA) from 2000-2016. We reviewed charts for demographics, PHOX2B genotype, ventilatory support, comorbidities, anesthetic and perioperative course. Endpoints were time to extubation or return to home ventilator settings, length of ICU stay and hospital stay.
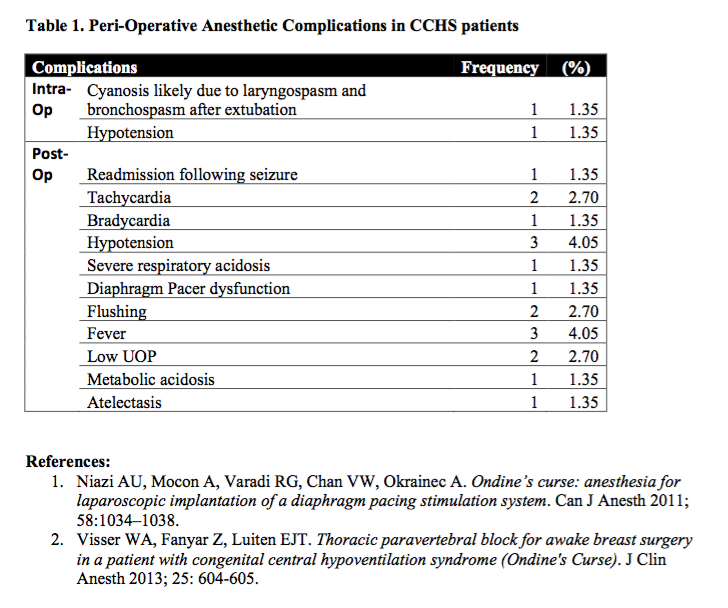
Results: Nineteen patients with a mean age of 6.9 years (42% males) underwent a total of 74 procedures in the study period (62% ENT, 10% dental, 10% GI, and 18% others). PHOX2B mutation was seen in 18 patients. Common comorbidities were Hirschsprung’s disease (32%), GERD (26%), G-tube dependence (21%) and cardiac pacemaker dependence (16%). At baseline, 14 patients were ventilator dependent during sleep: 7 used PPV via tracheostomy and 7 had diaphragmatic pacers. Airway management included LMA in 1 and ETT intubation in 21 cases. The mean times to extubation and discharge from hospital were 1.52 and 13.3 days, respectively. Interestingly, 22 cases received Midazolam as premedication with 2 requiring airway assistance in the preoperative area. Long-acting neuromuscular blockers (NMBs) were used in 24 cases of which only 17 were reversed. Intraoperative opiates were given in 32 cases, IV morphine (2) and IV fentanyl (29) and epidural morphine (1). There were 2 intra-operative and 18 post-operative adverse events (Table 1).
Discussion: Literature on optimal anesthetic care is lacking, existing mostly as case reports. As a referral center for CCHS, we present our anesthetic experience in these children. Anesthetic management is challenging with goals including avoidance of hypoxia, hypercarbia, acidosis, hypo or hypervolemia, and hypothermia while providing adequate anesthesia and pain control. Long acting opioids have profound respiratory depression and should be avoided. Regional techniques are excellent for post-op pain control. However, it is often difficult to use this as the primary anesthetic in pediatric population. Long acting NMBs should be appropriately reversed. [1-2] Premedication with benzodiazepines should be avoided due to the increased risk for apnea in an inappropriate setting; parental presence on induction should be considered. In conclusion, it is imperative for the anesthesiologist to have a good understanding of the condition and its associated comorbidities as well as secondary complications to achieve the best outcome.
Top