NM-241
IONM decision algorithm for improved safety in children with Hurler syndrome undergoing non-spine surgery: Our experience
Kandil A, Careskey M, Pettit C, Chesnut E, Buck D, Habeych M, Berry L, Leslie N, McAuliffe J, Chidambaran V
Cincinnati Children's Hospital, Cincinnati, Ohio, USA
Introduction: Patients with Hurler syndrome pose unique challenges to the anesthesiologist. Treatment with BMT has improved airway challenges; however, emerging evidence suggests that the spinal deformities in these patients remain a problem, and place them at increased risk for spinal cord ischemia during non-spinal surgeries (1). Presence of kyphotic beaks and stiff spines require increased attention to maintaining spinal cord perfusion in these patients (3). Thus, intraoperative neuromonitoring (IONM) is a useful modality for identifying and preventing irreversible SCI in these fragile patients. However, there are no established guidelines for instituting IONM for non-spine surgeries.
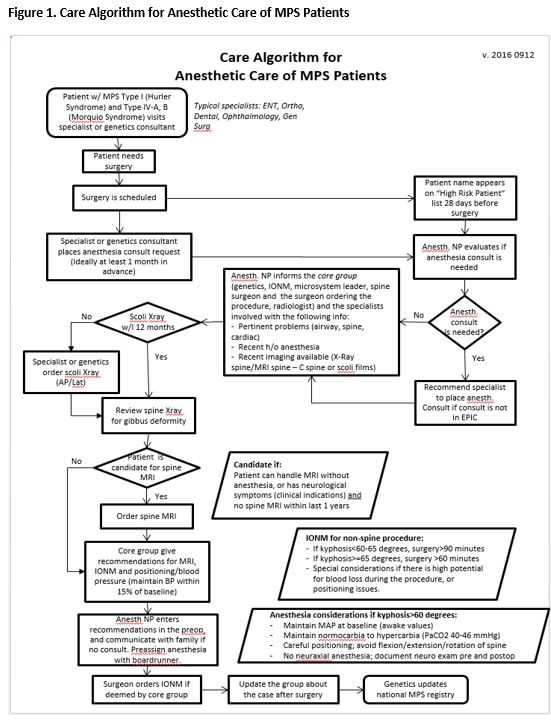
Methods: We held multidisciplinary meetings, reviewed cadaveric studies noting significantly increased intramedullary pressure with critical kyphotic angles (4), prior case reports and discussed the standard of care at other institutions to develop our own IONM decision algorithm for children with Hurler syndrome undergoing non-spine surgery. We implemented this algorithm through incorporation into the pre-anesthesia evaluation in EPIC. We present our experience with this algorithm and IONM for children with Hurler syndrome over the past year, with descriptives, modalities monitored, changes in IONM, and measures necessitated by IONM.
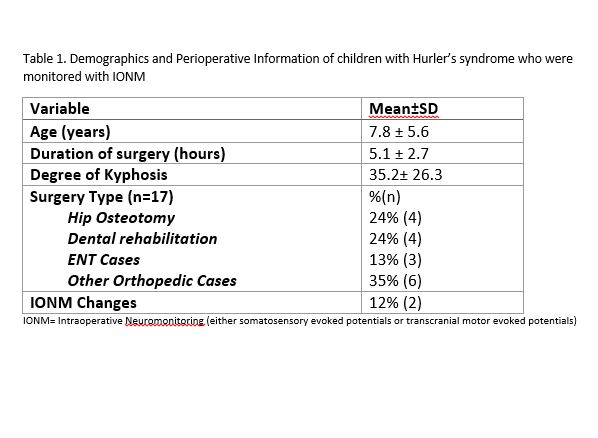
Results: The decision tree in the developed algorithm is dictated by degree of kyphosis from scoliosis films and surgical risk (duration, positioning and blood loss) (Fig 1). EPIC best practice alerts were instituted so anesthesia providers were aware of positioning and special care considerations (including avoiding neuraxial blocks). Based on this algorithm, IONM was instituted for 17 children with Hurler syndrome requiring non-spine surgeries. Details of these subjects are presented in Table 1. We detected changes in transcranial motor evoked potentials and somatosensory evoked potentials in 2 patients, for whom we intervened intraoperatively, mostly with blood pressure management and re-positioning, and prevented sustained injury to the spinal cord and upper extremity. None of these patients sustained neurological deficits.
Conclusion: Incorporation of a decision algorithm in the preoperative evaluation of children with Hurler syndrome, and use of IONM in properly selected patients adds to intraoperative patient safety and may prevent spinal cord injury.
REFERENCES
1) Pruszczynski B, et. al. Clin Orthop Relat Res.2015 Oct;473(10):3315-3320.
2) Tong CK, et. al. J Neurosurg Pediatr. 2012;9:608-12.
3) Othman Z, et. al. Spine. 2004;29:E258–E265.
4) Chavanne A, et. al. Spine. 2011 Sep 15;36(20):1619-26.
Top