NM-336
Intrathecal and superior hypogastric neurolytic block for intractable pediatric cancer pain
Carrie S, Morrill D, MacDonald J, Padua H, Berde C
Boston Children's Hospital, Boston, MA, United states
Pain due to pediatric cancer can generally be treated successfully with systemic analgesics and adjuncts per the World Health Organization analgesic ladder. In a small subset of patients with refractory pain or unmanageable side effects, there is a role for regional techniques involving infusion of local anesthetics and opioids. We describe a novel case in which two approaches to neurolytic block, a hyperbaric phenol intrathecal block as well as superior hypogastric phenol block were used to treat intractable perineal and pelvic pain in a pediatric oncology patient.
The patient is a 13 years-old female with severe perineal and pelvic pain secondary to a non-resectable metastatic embryonal rhabdomyosarcoma. Tumor filled the pelvis and a large chronically infected mass extended externally through the perineum. She had a colostomy, suprapubic cystostomy and required twice weekly wound care. She was confined to bed with debilitating pain despite numerous medication adjustments. Pain was judged to involve both thoracic and sacral visceral afferents and sacral (pudendal) somatic afferents. We elected a stepwise approach with a temporary intrathecal catheter and superior hypogastric neurolysis, followed later by a second combined neurolytic procedure.
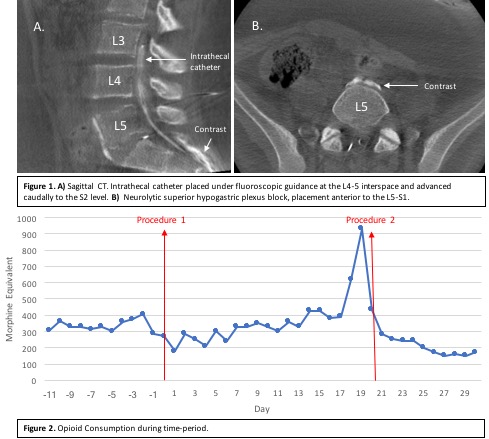
For the first combined procedure, we used Dyna-CT for needle guidance for superior hypogastric plexus anterior to the L5-S1 disc (Figure 1a), and 15ml of phenol 6% was injected. Next, an intrathecal catheter was placed under fluoroscopic guidance entering at the L4-5 interspace and advanced caudally to S2. (Figure 1b). For the second combined procedure, single shot superior hypogastric plexus phenol block and hyperbaric intrathecal phenol block were performed using fluoroscopic guidance.
After recovery from the first procedure, an intrathecal ropivacaine-hydromorphone infusion was initiated and confirmed to be effective in improving pain and alertness. Over the next 4 days, repeated doses of hyperbaric phenol 5.1% in dextrose 7% were injected via the catheter for sacral root neurolysis with the patient sitting upright, to a total volume of 4.5ml. After initial improvement, pain and opioid consumption increased dramatically two weeks later. The tumor continue to grow throughout this period and based on her consideration of goals of care, both neurolytic procedures were repeated as single shot injections.
Following these procedures, the patient reported significant improvement in her pain which was reflected in her opioids consumption (Figure 2). The mean opioid consumption before the first procedure was 339.9 mg morphine equivalents (ME) and 275.2 mg ME post procedure; pre-procedure 2, this increase to 449.5 mg ME and decreased to 223.7 mg ME after the second procedure.
In highly selected cases of localized intractable cancer pain, there may be a role for neurolysis. In this case, a multidisciplinary team worked closely together to devise a plan that suited the goals of care.
Top