NM-245
Age-dependent impact of pre-transplant ICU stay on mortality in heart transplant recipients
Sims T, Tumin D, Hayes D, Tobias J
Nationwide Children's Hospital, Columbus, Ohio, United states
Introduction: Heart transplantation (HTx) is definitive treatment for end-stage heart failure refractory to optimal medical management. Although severe illness requiring pre-transplant intensive care is a recognized risk for diminished post-transplant survival, recent studies have found surprising inconsistency in the association between pre-transplant intensive care unit (ICU) stay and HTx outcomes. Specifically, this association was absent in studies including adolescents and young adults, in contrast to studies that were limited to infants or included older adults. To clarify the significance of ICU stay as a risk factor for heart transplant outcomes, we aimed to define the age ranges in which ICU stay was predictive of survival after HTx.
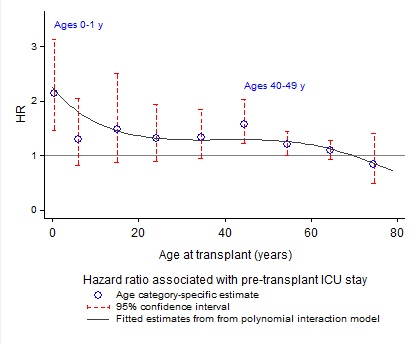
Methods: De-identified data were obtained on isolated first-time HTx performed in 2006-2016 from the United Network for Organ Sharing. Nine age groups (≤1, 2-11, 12-18, 19-29, 30-39, 40-49, 50-59, 60-69, and ≥70 y) were defined. The primary outcome was 1-year post-transplant mortality, and univariate Cox proportional hazard regressions estimated the hazard ratio (HR) associated with pre-transplant ICU stay in each age group. A multivariable Cox model interacting ICU stay with polynomial continuous patient age was used to estimate smooth change in the HR of ICU stay across patient age.
Results: The analysis included 24,207 patients (9% deceased within 1 year of HTx). On univariate analysis in each age group (Figure), ICU stay was most strongly associated with increased mortality hazard among infants (n=1,514; 70% in ICU; 12% 1-year mortality; HR=2.2; 95% CI: 1.5, 3.2; p<0.001) and patients ages 40-49 (n=3,234; 30% in ICU; 8% 1-year mortality; HR=1.6; 95% CI: 1.2, 2.0; p<0.001). Multivariable analysis confirmed maximal association of ICU stay with mortality among the youngest recipients, with gradual reduction of this risk at later ages.
Discussion: Our study established age variation in the association between ICU stay and survival after HTx, with this association being strongest among infants undergoing HTx. This may suggest opportunities for improving management of infants in the ICU prior to HTx, such as by using mechanical circulatory support in the ICU to optimize the clinical condition of these candidates prior to transplant. The stronger association between ICU stay and post-transplant survival in infants might also be explained by overall higher risk for post-transplant mortality among younger HTx candidates, especially children awaiting HTx for congenital heart disease; and age variability in the size matching and quality of transplanted donor hearts.
Conclusions: Pre-transplant ICU stay was a significant risk factor for post-HTx mortality in infants, but not older children. Among adults, ICU stay was especially associated with post-transplant mortality in early middle age.
Top