NM-376
The Impact of Trainees on Efficiency and Patient Outcomes for Pediatric Circumcisions: Residents vs. Fellows
Barry K, Baier A, Staffa S, Leahy I, Brustowicz R
Boston Children's Hospital, Boston, MA, USA
Background:
Teaching hospitals face competing priorities of training and educating students while maintaining efficient, quality, cost-effective care.1,2 However, level of trainee experience also mitigates degree of trainee impact on such measures.3 The goal of this study is to elucidate the impact of residents and fellows on efficiency measures and patient outcomes in a teaching hospital and outpatient setting.
Methods:
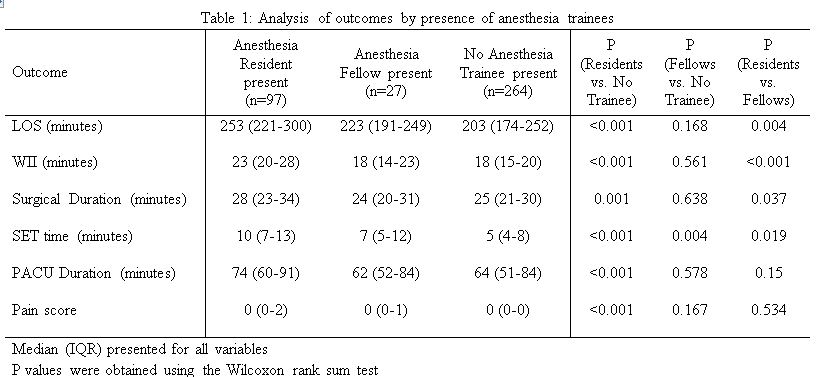
After IRB approval, all circumcisions performed at Boston Children’s Hospital and its Waltham, MA campus from 2016 to June of 2017 (n=388) were queried. Patients with ASA status >II, those undergoing multiple concurrent procedures and those with missing pain scores were excluded. Cases were categorized by the presence of either residents (n=97) or fellows (n=27). The impact of anesthesia trainees on Surgical End to Transport (SET) time, surgical duration, PACU duration, total Length Of Stay (LOS), Wheels In to Incision (WII) and pain score was calculated. The Wilcoxon rank sum test was used to compare the outcomes between groups. Significance was set at p<0.05.
Results:
Comparison of cases involving an anesthesia resident vs. cases without an anesthesia trainee demonstrated statistically significant longer LOS, surgical duration, WII, PACU duration, SET time, and higher pain scores. Cases with an anesthesia fellow had longer SET Time than cases with no anesthesia trainee. Cases with an anesthesia resident demonstrated longer WII, surgical duration, SET Time and LOS compared to cases with an anesthesia fellow. (See Table 1 for details)
Discussion:
When examining the efficiency parameters and patient outcomes, resident trainees demonstrated the greatest difference when compared to no anesthesia trainees. When comparing fellows to no anesthesia trainees, the differences were smaller, reflecting the fellows’ greater degree of experience. While the earlier cited study3 limited their comparisons to specific intraoperative events, the data presented here demonstrates that the entire perioperative experience is affected by the presence of trainees. This analysis was limited by its retrospective nature. Future analyses will quantify the fiscal impact of trainees on hospital costs.
Conclusion:
Providing efficient, quality care is more challenging when also training future healthcare providers.
References:
1. Overdyk FJ, Harve SC, Fishman, RL, Shippey F. Successful Strategies for Improving Operating Room Efficiency at Academic Institutions. Anesth Analg. 1998; 86: 896-906.
2. Welk B, Winick-Ng J, McClure A, Vinden C, Dave S, Pautler S. The impact of teaching on the duration of common urological operations. Can Urol Assoc J. 2016; 5: 172-176.
3. Eappen S, Flanagan H, Bhattacharyya N. Introduction of anesthesia resident trainees to operating room does not lead to changes in anesthesia-controlled times for efficiency measures. Anesthesiology. 2004; 99: 236-242.
Top