AIR-14
Significant Narrowing and Deviation of the Trachea in an Osteogenesis Imperfecta Type III Patient: Previously Unreported
1Dobish M, 2Budzinski J, 2Theroux M, 2Shah S, 2Averill L
1Thomas Jefferson University Hospital, Philadelphia, PA, USA; 2Nemours/Alfred I. duPont Hospital for Children, Wilmington, DE, USA
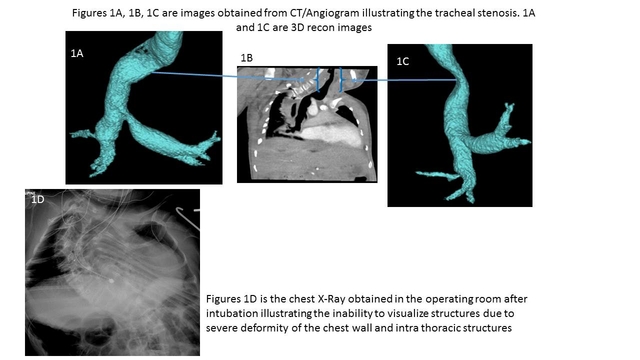
Case Report: A 19 year-old male with a diagnosis of Osteogenesis Imperfecta (OI) type III and severe thoracolumbar scoliosis presented for a T2-L4 spinal fusion. Due to the severity of the spinal curvature and the small thoracic cavity, the trachea was poorly visualized in preoperative chest X-ray (Figure 1A). On physical examination our patient was an alert, thin young man with pectus carinatum and limited neck movement. After induction with 4 mg/kg of propofol and 6% sevoflurane, hand ventilation became difficult and an oral airway was placed. Direct laryngoscopy was performed using a Macintosh #3 blade and a 6.5mm cuffed endotracheal tube (ETT) was passed through the vocal cords, but could not be advanced further. A 2.8 mm fiberoptic scope was placed through the ETT which revealed a severely deviated and torturous trachea past the thoracic inlet. Using the fiberoptic scope, the ETT was maneuvered past the deviation and positioned proximal to the carina. Pulse oximetry returned to 100% and an X-ray was taken to confirm tube position. At the end of the procedure, the trachea was extubated once the patient was awake and following commands. Postoperatively, we obtained a CT Angiogram which showed significant tracheal narrowing at the thoracic inlet (Figure 1A, B and C).
Discussion: While patients with OI are known to have upper airway difficulties due to kyphoscoliosis, limited neck mobility, and a prominent sternum, tracheal abnormality has not been described. Tracheal abnormalities including deviation, buckling and narrowing have been best described in lysosomal diseases, specifically Morquio syndrome (MS) (1). In MS, an enzyme deficiency causes accumulation of glycosaminoglycans (GAGs) in bones, cartilage, and soft tissues which impairs growth. This leads to deformities such as skeletal dysplasia, cord compression, and joint laxity. The prevailing theory is that differential growth rates between the trachea and the chest cavity results in a redundant, tortuous airway that buckles and deviates leading to severe airway distortion (2). In our patient, there was no direct tracheal compression by his kyphoscoliotic spine evident on CT/Angiogram. Similar to MS, OI patients are short stature and have a small thoracic cavity including a narrow thoracic inlet. This coupled with a kyphotic curve of the spine compromising the space available for the airways and major vessels may have impacted our patient. The severity and uniqueness of the tracheal abnormalities in this patient may be more prevalent as OI patients continue to live longer, and additional imaging studies may be required for detection.
Conclusion: In patients with OI, any suspicious finding in chest X-ray such as deviation or narrowing should be further evaluated for tracheal abnormality with CT or angiogram.
References 1,2: Tomatsu S, Averill LW et al. Obstructive airway in Morquio A Syndrome, the past, the present and the future. Mol Genet Metab 2015;(117):150-56.
Top