spa meeting reviews
Obstructive Sleep Apnea Panel
By Jorge Gálvez, MD
The Children’s Hospital of Philadelphia
University of Pennsylvania, Perelman School of Medicine
Dr. Shobha Malviya introduced an excellent panel that offered a timely update on the current state of anesthetic practice for children with obstructive sleep apnea (OSA) who also require sedation or general anesthesia. Charles Coté MD, FAAP (Massachusetts General Hospital, Boston) began the discussion by quantifying the additional anesthetic risks for patients with OSA. The CDC conducts ongoing surveillance of childhood obesity (http://www.cdc.gov/healthyyouth/obesity/facts.htm).
The most feared complication following sedation or general anesthesia for children with OSA is death due to respiratory depression or unrecognized upper airway obstruction during the recovery period. Dr. Coté identified several manuscripts that describe this phenomenon and quantified the risk. Goldman et al. conducted a survey of adult and pediatric otolaryngology surgeons which identified 51 cases of post-tonsillectomy deaths, four of which were associated with anoxic brain injury.1 Separately, Coté et. al. conducted analyzed data from a survey of members from the Society for Pediatric Anesthesia and data from the American Society of Anesthesiologists Closed Claims Project to evaluate post-tonsillectomy adverse events. The study identified 86 cases where death or permanent neurologic injury occurred.2 The adverse events described include both hemorrhage and post-operative respiratory complications. However, the incidence of respiratory complications due to medications may be under-reported and under-recognized. The authors call for additional research and validation of assessment tools to identify high-risk patients who may not be safely managed on an outpatient basis following administration of general anesthesia or sedation.
Article quote: “Deaths or neurologic injury after tonsillectomy due to apparent apnea in children suggest that at least 16 children could have been rescued had respiratory monitoring been continued throughout first- and second-stage recovery, as well as on the ward during the first postoperative night.”2
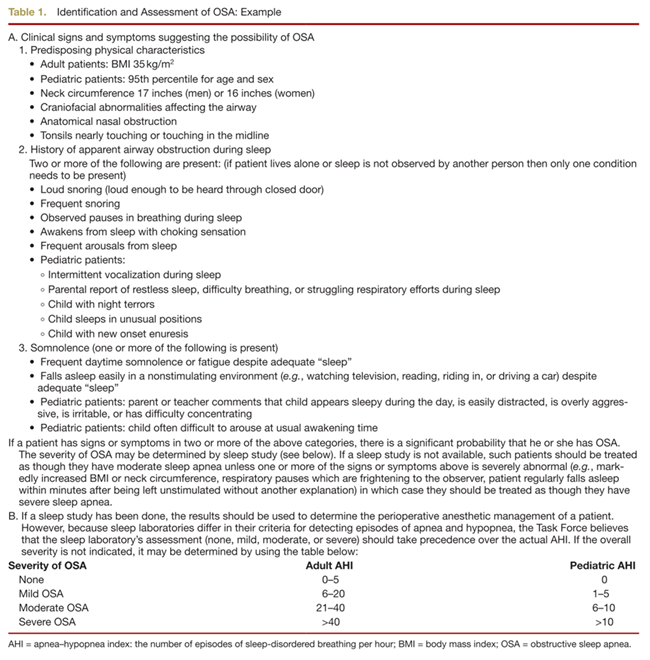
The presentation from Drs. Coté, Brown and Green also reviewed relevant data from a recent Anesthesiology article on “Practice Guidelines for the Perioperative Management of Patients with Obstructive Sleep Apnea” which was updated by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea.3 Table 1 in the manuscript (attached) provides a reference guide for history and physical evaluation to characterize individuals with OSA as well as a reference table for sleep study results for adults and children who may have OSA. Furthermore, recent guidelines from the American Academy of Otolaryngology- Head and Neck Surgery Foundation were reviewed. This document suggests that children with meeting the following criteria may be at increased risk and routine polysomnography prior to tonsillectomy should be performed:
-
Obesity
-
Down syndrome
-
Craniofacial abnormalities
-
Neuromuscular disorders
-
Sickle cell disease
-
Mucopolysachharidoses
The guidelines also recommend routine overnight observation of children experiencing severe OSA (apnea-hypopnea index of 10 or more obstructive events per hour or an oxygen saturation index of 80%, or both) as well as age less than three years.4 Dr. Coté also suggested exercising caution if there are adverse social conditions such as an unreliable support system at the patient’s home or patients who are geographically distant from emergency care services.
Karen Brown, MD (Montreal Children's Hospital, Montreal) then focused on the relationship between opioid exposure and respiratory depression particularly in children. She presented evidence demonstrating that children with known OSA and oxygen desaturation have decreased opioid requirements following tonsillectomy.5 She described a protocol tailored to anesthesiologists with the goal of reducing the intraoperative use of opioids for post-tonsillectomy analgesia which demonstrated a significant reduction of post-operative respiratory depression without affecting pain score outcomes between the group that received higher or lower doses of morphine.6 She postulated that if there is an increase in opioid sensitivity in patients with OSA, there may also be an increase in opioid-induced respiratory depression. Otherwise, why would children continue to die following tonsillectomy?
Given the resources required to make polysomnography available to all patients who require it are not realistic, Dr. Brown explored possible alternatives. In particular, home oximetry may be a potential solution when polysomnography is not feasible.7 Home oximetry simply requires a pulse oximetry study overnight and evaluation of the tracing for frequency and depth of desaturations. Clinical observations and evaluation for severity of OSA are not adequate and may have low specificity and sensitivity.8
Dr. Brown and Glenn E. Green, MD (CS Mott Children’s, Ann Arbor) both suggested active discussion of non-opioid analgesic techniques for patients with suspected or known OSA. The role of non-steroidal anti-inflammatory analgesics for tonsillectomy was briefly discussed and highlighted variations in practice across the country and world. Some centers are routinely using NSAIDS such as ibuprofen and even ketorolac while others are not using them routinely.
In summary, Dr. Brown suggests that children and adults with severe OSA have a heightened sensitivity to opioids. The risk could be mitigated with adequate pre-operative testing as well as monitoring for post-operative respiratory adverse events. If testing is unavailable, clinicians must evaluate the apneic threshold and opioid sensitivity on a case-by-case basis, running the risk that patients may have prolonged emergence or post-operative respiratory adverse events.
Audience question highlights:
Role of formal evaluation for OSA? Sleep polysomnography v. night pulse oximetry?
-
10-fold price difference between sleep polysomnography and home night oximetry
-
Clinical acumen is at best a coin-toss. Studies have demonstrated death due to respiratory depression following tonsillectomy.
-
Clinical criteria may not be sufficient. A test may be indicated, such as sleep polysomnography or home pulse oximetry.
What is the role of dexmedetomidine in patients with OSA?
-
Children who may exhibit airway obstruction during normal sleep will also likely exhibit airway obstruction with dexmedetomidine-induced sedation.
How do you approach children with suspected OSA who have not been tested?
-
If appropriate, administer 0.5mcg/kg of fentanyl to a spontaneously breathing child. If the respiratory rate decreases by 50% or more, the patient may be very sensitive to opioids.
Pain management alternatives
-
Surgeon’s perspective: Each study has demonstrated more hemorrhage with ketorolac, even if not statistically significant. Small things can make a big difference if you have a low rate of hemorrhage. Despite this data, Dr Green has been persuaded to prescribe ibuprofen.
Reference:
- Goldman JL, Baugh RF, Davies L, Skinner ML, Stachler RJ, Brereton J, Eisenberg LD, Roberson DW, Brenner MJ. Mortality and major morbidity after tonsillectomy. Laryngoscope 2013;123:2544–53.
- Coté CJ, Posner KL, Domino KB. Death or neurologic injury after tonsillectomy in children with a focus on obstructive sleep apnea: Houston, we have a problem! Anesth Analg 2014;118:1276–83.
- Bachenberg KL, Benumof JL, Diego S, Caplan R a, Connis RT, Cote CJ, Nickinovich DG, Prachand V, Ward DS, Weaver EM, Ydens L, Fe S, Yu S, Highway NN, Ridge P. Practice Guidelines for the Perioperative Management of Patients with Obstructive Sleep Apnea. 2006:1081–93.
- Roland PS, Rosenfeld RM, Brooks LJ, Friedman NR, Jones J, Kim TW, Kuhar S, Mitchell RB, Seidman MD, Sheldon SH, Jones S, Robertson P. Clinical Practice Guideline: Polysomnography for Sleep-Disordered Breathing Prior to Tonsillectomy in Children. Otolaryngol -- Head Neck Surg 2011;145:S1–15.
- Brown K a, Laferrière A, Lakheeram I, Moss IR. Recurrent hypoxemia in children is associated with increased analgesic sensitivity to opiates. Anesthesiology 2006;105:665–9.
- Raghavendran S, Bagry H, Detheux G, Zhang X, Brouillette RT, Brown K a. An anesthetic management protocol to decrease respiratory complications after adenotonsillectomy in children with severe sleep apnea. Anesth Analg 2010;110:1093–101.
- Horwood L, Brouillette RT, McGregor CD, Manoukian JJ, Constantin E. Testing for pediatric obstructive sleep apnea when health care resources are rationed. JAMA Otolaryngol Head Neck Surg 2014;140:616–23. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24851855.
- Constantin E, Tewfik TL, Brouillette RT. Can the OSA-18 quality-of-life questionnaire detect obstructive sleep apnea in children? Pediatrics 2010;125:e162–8.