Meeting Reviews
SPA Session I Review: Neurons, Needles, and Networks: Modulation Through the Ages
 By Chris D. Glover, MD, MBA
By Chris D. Glover, MD, MBA
Texas Children’s Hospital
This review covers the first session of the annual meeting aptly titled Neurons, Needles, and Networks: Modulation Through the Ages, which was moderated by Jennifer K. Lee, MD. The lectures covered in this review provided an update on anesthesia for neurosurgical care and the evidence behind acupuncture in pediatric anesthesia practice.
Sulpicio Soriano, MD, FAAP (Boston Children’s Hospital) presented a fantastic review and update in the field of neuroanesthesia. Dr. Soriano first reviewed mortality data for neurosurgical patients as well as their relative academic performance. While mortality in pediatric patients can approach 1.5%; neurosurgical patients, especially those with hydrocephalus and those undergoing craniotomy, can have significantly increased risk of death with rates approaching 19%. The academic performance for these children usually lags behind their peers.
When discussing cerebral autoregulation and cerebral perfusion in pediatrics, Dr. Soriano specifically pointed out the need to reassess the lower limit of autoregulation while also recognizing that premature neonates have alterations in autoregulation. Brady et al (Fig. 1) points out the readily apparent lower limit noted in pediatrics and Tsuji (Fig. 2) pointed out the autoregulatory variance that can occur in premature neonates [1,2]. Dr. Soriano also covered recent data on noninvasive blood pressures, which revealed children with regional anesthesia had minimal systolic pressures that were higher when compared to children undergoing general anesthesia.
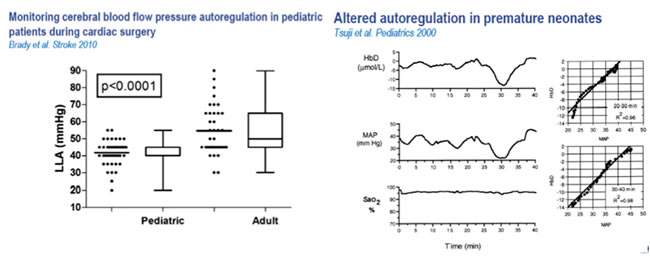
Figures 1 and 2
Caution should still be practiced however, before assuming that these findings are without sequelae. Dr. Soriano pointed out in the lecture that significant drops in systolic and diastolic blood pressure resulted in cerebral desaturation and hypoperfusion that could be causally related to general anesthesia exposure and propofol / remifentanil exposure (Fig 3). It was especially concerning given the findings by Vanderhaegen (Fig 4) pointing to an extended drop (>30 minutes) in mean arterial pressure following propofol administration [3]. These effects are potentially manifested by case reports of infantile postoperative encephalopathy following general anesthesia as reported by McCann [4]. All of the children were under 48 wks PCA with surgical duration >120 minutes with the majority of children exhibiting systolic blood pressures <60 mm Hg. Only 11% of the measured SBP values were outside one standard deviation for defined hypotension. Observations from this study specifically highlight the lack of evidence-based recommendations on the lower limits of adequate SBP and end-tidal carbon dioxide in anesthetized infants which should be taken into consideration in care delivery.
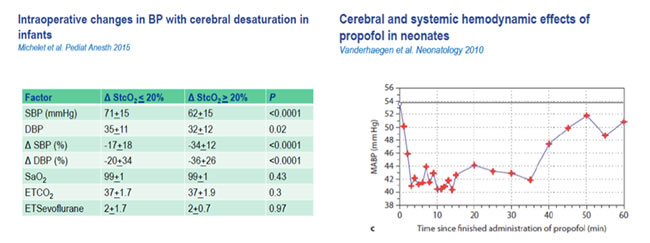
Figures 3 and 4
Dr. Soriano then transitioned to providing an update on reviewing blood-sparing techniques. A particularly compelling statistic correlated the amount of blood transfused in noncardiac surgery to the 30-day mortality rate. Children receiving >20 ml/kg of blood products had mortality significantly higher than matched controls. Subgroup breakdown revealed children receiving 40-59 ml/kg of blood products had a mortality rate 5X matched controls [6]. While traditional methods at limiting blood loss have been cited, Dr. Soriano rightly pointed out that the utility of these methods (hemodilution, allogenic blood transfusion, and induced hypotension) seems largely anecdotal. Literature does emphasize the use of antifibrinolytics regardless of type. When compared to placebo, tranexamic acid decreased blood loss and decreased amount of blood transfused in a statistically significant way [7]. While seizures have been classically linked to high dose antifibrinolytic exposure, Dr. Soriano cited a recent paper for cranial vault reconstruction where the incidence of seizures occurred at similar rates across cohorts.
When talking about predictors of morbidity following neurosurgery, Dr. Soriano began this portion of the lecture on advances within the field of neurosurgery. Advances such as endoscopic third ventriculostomy, endoscopic strip craniectomy, and MRI guided laser ablation for seizure focus all provide the potential for decreased blood loss and enhanced recovery. Regardless of approach, the point driven home seems to be that endoscopy can give a false sense with regard to risk profile in the perioperative period. Dr. Soriano further emphasized patient and procedure specific risk factors that should give anesthesia providers a way to identify those with potential for complicated recovery. These factors include:
- Weight <10kg
- >60 ml/kg of packed RBC exposure
- ASA status 3 or 4
- The use of intraoperative hemostatic products
- The nonuse of an antifibrinolytic
In conclusion, Dr. Soriano emphasized the need for continued vigilance in the face of surgical advancement in neurosurgical care. Hypotension and hypoxia remain significant predictors for poor outcomes and should be avoided at all costs.
Shu-Ming Wang, MD (University of Connecticut) covered the fascinating potential of acupuncture in pediatric anesthesia. Dr. Wang defined the practice of acupuncture as application of various physical stimulations to specific points on the body surface to promote physiologic balance and healing.
Dr. Wang started her lecture discussing efficacy data for acupuncture for craniotomy. 56 citations are noted on literature search from 1972 to 2015 [8]. Acupuncture provided statistically significant benefits in the following ways when used as part of the anesthetic plan:
- Reduced volatile anesthetic need
- Shortened time to extubation
- Improved postoperative patient recovery
- Reduction in plasma levels of a brain injury marker
- Reduction in PONV
Emphasizing the potential of this treatment method in postoperative nausea and vomiting, Dr. Wang again presented data on the P6 stimulation covering 40 trials and over 4800 patients [9]. The P6 acupressure point called Nei Guan is located three finger breadths below the wrist and between the two tendons on the inner forearm. Stimulation when compared to placebo resulted in:
- Reduced nausea
- Reduced vomiting
- Reduced need for antiemetic therapy
- Non-inferiority when compared to antiemetics
Another compelling concern for pediatric anesthesiologists is emergence delirium (ED) and Dr. Wang points to the potential of the HT-7 acupressure point in decreasing ED incidence. This point is located at the wrist crease, on the radial side of the flexor carpi ulnaris tendon.
Pain, or rather the reduction of pain, in the perioperative period has also been studied via the use of acupuncture. The meta-analysis points to the inclusion of acupuncture as an adjunct in decreasing pain through the perioperative period [10]. In pediatrics, Dr. Wang pointed out a small randomized controlled trial comparing acupuncture to sham procedure in those undergoing tonsillectomy. There were no significant differences in the amount of opioid medications administered or total postanesthesia care unit time between the two cohorts. Patients but not parents noted significant improvements in pain control. Oral intake improved significantly in the acupuncture group [11].
Dr. Wang finished her lecture by going over the data pointing to the efficacy of acupuncture in mitigating postoperative ileus. Again, the data seems to slightly favor use of acupuncture in patients at risk for development of ileus in the perioperative period through the use of acupressure at the ST 36 and ST 37 acupressure points.
While there seems obvious benefit in incorporating acupuncture in practice, Dr. Wang mentioned some inherent obstacles to widespread utilization; namely the time consuming nature in developing the requisite skills to place this intervention timely, delayed onset of intervention, and lack of financial remuneration for this technique when compared to those in current practice. Regardless of these potential barriers, the potential of this technique in pediatric anesthesia warrants further exploration.
- Brady, K.M., et al., Monitoring cerebral blood flow pressure autoregulation in pediatric patients during cardiac surgery. Stroke. 2010 Sep;41(9):1957-62.
- Tsuji M., et al., Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. JJ.Pediatrics. 2000 Oct;106(4):625-32.
- Michelet, D., et al., Intraoperative changes in blood pressure associated with cerebral desaturation in infants. Paediatr Anaesth. 2015 Jul;25(7):681-8.
- Vanderhaegen, J., et al., Cerebral and systemic hemodynamic effects of intravenous bolus administration of propofol in neonates. Neonatology. 2010 Jun;98(1):57-63.
- McCann, M.E., et al., Infantile postoperative encephalopathy: perioperative factors as a cause for concern. Pediatrics. 2014 Mar;133(3):e751-7. 6. Relationship between transfusion volume and outcomes in children undergoing noncardiac surgery.
- Goobie, S.M., et al., Relationship between transfusion volume and outcomes in children undergoing noncardiac surgery. Transfusion. 2016 Oct;56(10):2487-2494.
- Goobie, S.M., et al., Efficacy of tranexamic acid in pediatric craniosynostosis surgery: a double-blind, placebo-controlled trial. Anesthesiology. 2011 Apr;114(4):862-71.
- Asmussen, S., et al., Effects of Acupuncture in Anesthesia for Craniotomy: A Meta-Analysis. J Neurosurg Anesthesiol. 2017 Jul;29(3):219-227.
- Lee, A., et al., Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2015 Nov 2;(11):CD003281.
- Wu, M.S., et al., The Efficacy of Acupuncture in Post-Operative Pain Management: A Systematic Review and Meta-Analysis. PLoS One. 2016 Mar 9;11(3):e0150367.
- Tsao, G.J., et al., Intraoperative acupuncture for posttonsillectomy pain: a randomized, double-blind, placebo-controlled trial. Laryngoscope. 2015 Aug;125(8):1972-8. doi: 10.1002/lary.25252.