Improving the Safety of Pediatric Anesthesia in Low And Middle-Income Countries Through Education: The Safe PAEDS Experience
Sung Choi, MD, MALD
CA-3 anesthesiology resident, Saint Elizabeth's Medical Center, and Clinical Associate, Tufts University School of Medicine, Boston, MA
Faye Evans, MD, FAAP
Chair, SPA Committee on International Education & Service
Senior Associate, Boston Children’s Hospital
Assistant Professor, Harvard Medical School, Boston MA
The Lancet Commission on Global Surgery estimates that five of the world’s seven billion people do not have access to safe, affordable anesthesia and surgical care when needed.1 In addition, great disparity exists with up to 70% of the world’s population living in the poorest countries yet accounting for only 25% of surgical operations performed worldwide.2 Not only do these countries not have access to anesthesia and surgical care, the care may be deficient when compared to anesthetic care in high-income countries (HIC).3 In fact, countries higher on the Human Development Index (HDI - a United Nations composite statistic based on life expectancy, literacy, education, and per-capita income that ranks countries into tiers of human development)4 have actually experienced a decrease in overall perioperative mortality, as well as mortality specifically associated with anesthesia. For those countries with a lower HDI, specifically low and middle-income countries (LMICs), anesthesia-related mortality has actually increased.5
Regardless of setting, pediatric surgical patients face more risk of harm during the perioperative period. Observational data on adverse outcomes have shown that infants between one month and one year of age have an approximately four times higher risk of anesthesia-related cardiac arrest than do children one to 18 years of age, and infants younger than one month have an approximately 6 times higher risk of cardiac arrest than do infants between one month and one year of age.6,7,8
Given that as much as 40% of a LMIC country’s population can be under the age of 18,9 and it is estimated that 85% of these children will require surgery by the age of 15,10 more attention paid to the provision of safe pediatric anesthetic care, in parallel with improving the quality of anesthetic care overall, is imperative. This is a big challenge in LMICs as, even in high HDI countries, anesthetic care for very young children in rural areas may not meet the standard achieved in more affluent regions of those countries.11
Providers in LMICs face many obstacles to providing optimal care for children. The origin of this problem is multifactorial and includes many failures at the systems level such as lack of adequate monitoring and equipment, and infrastructural problems with electricity, oxygen and water deficiencies.12,13,14 Beyond material needs, a properly trained physician or non-physician anesthesia provider is often not available to care for the patients during and after surgery. A recent survey of the global anesthesia workforce found that almost 50% of the 153 countries studied have fewer than five physician anesthesia providers per 100,000 population, with some countries reporting zero physician anesthesia providers. (Figure 1) Even when non-physician anesthesia providers were included, very few countries had over 5 per 100,000 population.15 For the few anesthesia providers that do exist, there are limited opportunities for continuing education or mentorship as they often work in isolation under very challenging conditions.
Recognizing the need for pediatric-specific anesthetic training in LMICs, the Association of Anaesthetists of Great Britain and Ireland (AAGBI) in partnership with the World Federation of Societies of Anaesthesiologists (WFSA) developed the Safer Anaesthesia from Education (“SAFE”) training course, SAFE Paeds. The goal of this course is to provide refresher training for both physician and non-physician anesthesia providers working in resource-limited settings on the fundamentals of pediatric anesthesia, and is specifically targeted at those who expect to be, or are already, engaged in the daily delivery of anesthetic care to children.
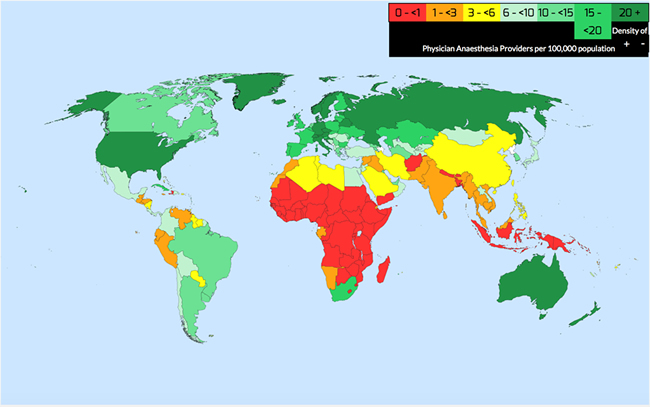
Figure 1. WFSA Global Anesthesia Workforce Survey16
SAFE Paeds is designed as an “off the shelf” modular three-day course emphasizing the principles of safe care for children including assessment, vigilance, and competence in essential skills. The course was developed using adult learning principles with very few didactic lectures and consists of primarily of small-group breakout sessions comprised of case scenarios, discussions and skills stations. Topics include:
- Preoperative assessment of the pediatric patient
- Airway management in children
- Common elective and emergency conditions in children
- Neonatal and Pediatric Life Support
- Pain Management
- Pediatric Trauma and Resuscitation

SAFE faculty member demonstrating pediatric airway management techniques
Monitoring and evaluation are an integral part of the course. Knowledge and skills are assessed by pre- and post-course tests. Plans for longer-term follow-up are under development.
Course participants are identified by local anesthesia leaders, often in cooperation with the national anesthesia society, and are invited to attend. In order to promote sustainability by local providers, each SAFE Paeds course includes a one-day ‘Train-the-Trainer’ course (TTT) for potential local course leaders to teach them the skills necessary to utilize the information learned in the course to train others in the future.

Every SAFE course includes a ‘Train-the-Trainer’ (TTT) component incorporating the goals of the SAFE curriculum and methods to optimize adult learning
Participation in the course is typically at little or no cost to the learner, and equipment purchased or donated to run the initial course in a country is typically donated to the local anesthesia society and left in-country for use on future courses and other educational programs.
From 2014 – 2017, SAFE Paeds courses have been run in nine countries worldwide with over 750 anesthesia providers trained. Countries include Bangladesh, Benin, Ethiopia, India, Madagascar, Malawi, Uganda and Zambia. Upcoming courses are planned for Kenya and Cameroon. In addition, the Society for Pediatric Anesthesia, in collaboration with the WFSA, and the Guatemalan Anesthesia Society recently hosted the first SAFE Paeds course in Latin America in Guatemala City this past December. (Editorial Note: A report of this course will be included in the next edition of SPAnews)
In addition to knowledge transfer, a fundamental goal of the SAFE Paeds course is to support the local anesthesia community by promoting cooperation and networking among a diverse group of anesthesia providers regardless of age, experience and anesthesia training. Per report, (via personal communication with Dr. Susane Nabulindo, Kenya) these courses have been instrumental in building the foundations for regional, national and even international networking opportunities for anesthesia providers of all training backgrounds with specific interest in pediatric anesthesia.

Course delegates receive ample feedback and instruction on fundamental life support skills.

The future of pediatric anesthesia in Ethiopia: Anesthesiology residents from Black Lion Hospital in Addis Ababa, Ethiopia.
The challenges going forward are common to many medical “short courses,” specifically, evaluating the definitive impact in terms of efficacy and improved outcomes as these are very difficult to measure. Ensuring skills retention and long-term knowledge are obstacles found even in very robust medical educations systems. Finally, it is imperative to constantly reassess the relevance of teaching materials. For example, during the March 2017 Safe Paeds course run in Addis Ababa, Ethiopia, a significant number of the course delegates had access to only intravenous meperidine for analgesia, rendering discussions on medications such as morphine or fentanyl less applicable to their daily practice.
Conclusion
In March of 2014, the American College of Surgeons published a document outlining principles regarding resource standards, quality-improvement and safety processes, data collection, and a verification process that ultimately resulted in the development of the Children’s Surgery Verification (CSV) Program.17 This program aims to classify surgical centers in the United States, as has been done with trauma centers for decades, according to the resources available, recognizing that many pediatric surgical patients have specific medical, emotional and social care requirements that may only be met in a specialized environment. The provision of safe pediatric anesthesia care was recognized as a critical component of this program.
We are far from this level of specialization in most LMICs, where access to surgery at all is considered a luxury, but it is critical to recognize the specific nature and challenges faced by those who provide anesthetic care for infants and children in remote areas of the world. SAFE Paeds is a part of a growing network of global anesthesia initiatives whose goals are to improve local capacity and ownership of anesthetic standards and professionalism in developing countries. It recognizes the principles of developing an effective curriculum for anesthesia training in developing countries that includes sustainable efforts focused on reducing the need for external support, emphasis on patient safety and improving outcomes.
References:
Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015; 386:569-624.
Weiser TG, Regenbogen SE, Thompson KD et al (2008) An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 372:139–144.
Ouro-Bang’na Maman AF, Tomta K, Ahouangbevi S, Chobli M. Deaths associated with anaesthesia in Togo, West Africa. Trop Doct 2005; 35: 220–22.
Human Development Report 2016. New York: United Nations Development Program, 2016. Available at: http://hdr.undp.org/en/2016-report. Accessed Aug 20th, 2017.
Bainbridge D, Martin J, Arango M, Cheng D, for the Evidence- based Peri-operative Clinical Outcomes Research (EPiCOR) Group. Perioperative and anaesthetic-related mortality in developed and developing countries: a systematic review and meta- analysis. Lancet. 2012; 380:1075–81.
Cohen MM, Cameron CB, Duncan PG. Pediatric anesthesia morbidity and mortality in the perioperative period. Anesth Analg. 1990;70(2):160–167
Gobbo Braz L, Braz JR, Módolo NS, do Nascimento P, Brushi BA, Raquel de Carvalho L. Perioperative cardiac arrest and its mortality in children. A 9-year survey in a Brazilian tertiary teaching hospital. Paediatr Anaesth. 2006;16(8):860–866
Flick RP, Sprung J, Harrison TE, et al. Perioperative cardiac arrests in children between 1988 and 2005 at a tertiary referral center: a study of 92,881 patients. Anesthesiology. 2007;106(2):226–237.
World Bank. Population ages 0-14 (% of total). Retrieved from http://data.worldbank.org/indicator/SP.POP.0014.TO.ZS. Accessed Aug 20th, 2017.
Bickler SW, Sanno-Duanda B. Epidemiology of paediatric surgical admissions to a government referral hospital in the Gambia. Bull World Health Organ, 2000; 78: 1330–36.
de Graaff JC, Sarfo MC, van Wolfswinkel L, van der Werff DB, Schouten AN. Anesthesia-related critical incidents in the perioperative period in children; a proposal for an anesthesia-related reporting system for critical incidents in children. Paediatr Anaesth. 2015;25(6):621–9.
Walker IA, Obua AD, Mouton F, Ttendo S, Wilson IH. Paediatric surgery and anaesthesia in south-western Uganda: a cross-sectional survey. Bull World Health Organ. 2010 Dec 1;88(12):897–906.
Bösenberg, A. Neonatal anesthesia with limited resources. Paediatr Anaesth 2014, 24:98–105.
Ivani, G., Walker, I., & Enright, A. Safe perioperative pediatric care around the world. Paediatr Anaesth. 2012 Oct;22(10):947-51
Kempthorne, P., Morriss, W. W., Mellin-Olsen, J., & Gore-Booth, J. The WFSA Global Anesthesia Workforce Survey. Anesth Analg 2017 Sep;125(3):981-990.
World Federation of Societies of Anesthesiologists. World Anaesthesiology Workforce. Available at http://www.wfsahq.org/workforce-map. Accessed August 26th, 2017. (Additional information on the method of data gathering can be found in reference 13, noted above.)
Oldham, K. Optimal Resources for Children’s Surgical Care. J Pediatr Surg. 2014 May;49(5):667-77.