Pediatric Anesthesiology 2018 Reviews
Friday Session II
Regional Romance: Controversies Surrounding Regional Techniques
Reviewed by Franklin Chiao, MD
Assistant Professor of Anesthesiology
New York Presbyterian Medical Center
Weill Cornell Medical College
"Regional Romance" covered some exciting topics. First, it focused on analgesia for pectus excavatum repair. The second topic addressed the controversy regarding caudal for hypospadias surgery and introduced the pudendal block technique. Lastly, there was a lively debate about pediatric regional anesthesia placement in asleep versus awake children.
Joseph Cravero, MD (Boston Children’s Hospital) was the first speaker. The NUSS procedure is one of the most painful surgeries as a metal bar is placed in the chest to expand the anterior chest wall to correct pectus excavatum. Data was collected and analyzed through the Society for Pediatric Anesthesia Improvement Network (SPAIN). It is a multicenter prospective collaborative group that was started in 2014. One paper was discussed "Postoperative management of patients following the Nuss procedure: A survey of practice". A survey with 51 questions was sent to 108 international pediatric hospitals. 58 institutions completed the survey.
Results showed 91% of centers use thoracic epidural and 27% add PCA to this. Thoracic levels T4 to T6 were the most commonly used level of placement for a duration of three days. 16% had stopped using epidurals partly due to negative case reports. Multimodal technique was extremely common as diazepam and gabapentin were used in 30% of cases.
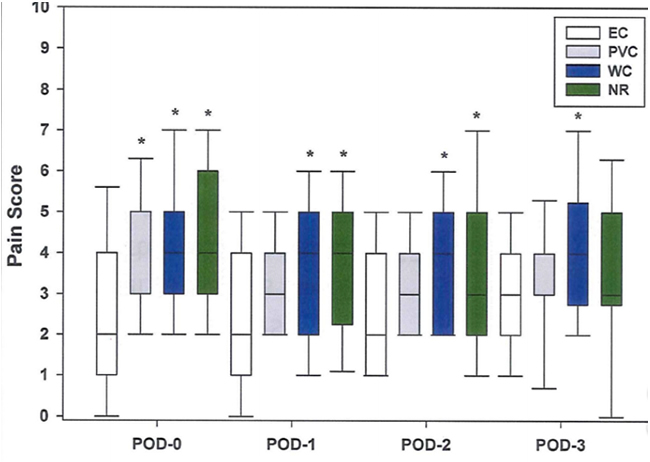
As shown in this figure, epidural catheter (EC) provided superior pain control the first two days postoperatively. More epidural patients needed a Foley though, and discharge showed a trend toward a longer stay.
Sean Flack, MBChB, FCA, (Seattle Children's Hospital) then gave an enlightening lecture on hypospadias pain management. He went over risk factors for fistula post-operatively. These included severity of hypospadias, proximal shaft location, surgical skill, and epinephrine use. There is controversy whether caudal causes fistula from penile engorgement as recent papers have shown both positive and negative factors. This body of research still lacks high quality studies, as there are no randomized prospective controlled trials. In addition, regional anesthesia is generally considered to improve wound healing and has been used for limb ischemia treatment.
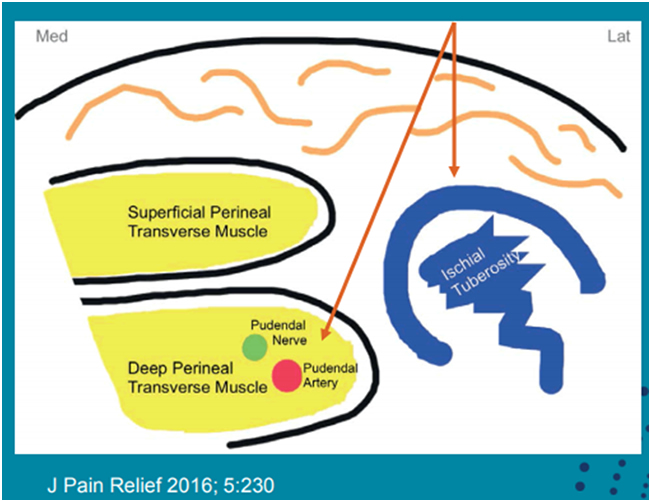
In addition to penile block and caudal analgesia, pudendal block has emerged as a promising alternative. The pudendal nerve is derived from 2nd - 4th sacral ventral rami and travels in the pudendal (Alcock’s) canal. Branches include the inferior rectal, perineal and dorsal nerve of the penis/clitoris. This technique is performed with either landmark, nerve stimulation or ultrasound techniques. All techniques describe patient in the lithotomy position, identification of the ischial tuberosity, with needle tip in ischiorectal fossa, negative aspiration, and injection of 0.25mL/kg each side without epinephrine.
The landmark technique is performed by walking the needle off the ischial tuberosity (IT), piercing the sacrococcygeal ligament, and then injecting as shown in this diagram.
The nerve stimulator technique is also commonly used. Using a perpendicular trajectory, immediately medial to the IT, with 3mA, at 2Hz, one will first see external anal sphincter contraction followed by perineal muscle contraction. Up and down penile movement confirms that the needle tip is in the correct position but may only be elicited in 20% of patients. Dr. Flack described the ultrasound technique as well. An out of plane technique, with color doppler is used. Care is taken to see the needle tip, and a test injection is given.
Drs. Tarun Bhalla MD, MBA (Nationwide Children's Hospital) and Peter Marhofer MD (Medical University of Vienna, Vienna, Austria) presented a pro-con debate about asleep or awake regional anesthesia in children. Logically, an immobile child has less risk for injury because a moving and uncooperative patient is a challenge to block. In addition, awake patients are not reliably able to indicate a neural injury as per an ASRA Practice Advisory that was referenced. An additional paper with 4200 patients with lumbar epidural showed no neural complications. Moreover, PRAN research showed 18,000 asleep caudal block placements with no cases of temporary or permanent injury.
The argument for awake/light sedation regional anesthesia placement revolved around the avoidance of airway intervention/intubation as the child can breathe spontaneously. There is also the avoidance of side effects from general anesthesia, and quicker enteral nutrition postoperatively. When done well, awake regional requires less OR time.