Pediatric Anesthesiology 2018 Reviews
Friday Session IV
Pediatric Surgery and Anesthesia Capacity Building Model in Low and Middle-Income Countries
 Reviewed by Jenna Helmer Sobey, MD
Reviewed by Jenna Helmer Sobey, MD
Vanderbilt Children’s Hospital
Session IV on Friday this year focused on the current challenges and advances in the care of pediatric surgical patients in low and middle income countries, including a view from a surgeon’s perspective and advice on how to participate responsibly with global health initiatives as an anesthesiologist. In the second lecture, Mark Newton, MD (Vanderbilt Children’s Hospital) gave a powerful presentation titled “Pediatric Surgery and Anesthesia Capacity Building Model in Low and Middle Income Countries.”
Dr. Newton moved to Kenya over 20 years ago from the US after completing his training in pediatric anesthesia at Denver Children’s Hospital. He lives in Kijabe, Kenya for 70% of the year and practices as a Professor in the Department of Pediatric Anesthesia at Vanderbilt Children’s Hospital for the other 30% of the year.
Dr. Newton began his talk by discussing the landscape of anesthesia care for children in low-resource settings. He briefly outlined some of the 2015 Lancet Commission on Global Surgery findings, including the fact that 5 out of 7 individuals globally do not have access to safe and affordable surgery and anesthesia. In addition, the Lancet Commission developed a benchmark of 5,000 operations/100,000 population so that our interventions have a measure of success, a target. He pointed out that although there has been tremendous progress in surgical services delivered in Eastern Sub-Saharan Africa (a 112% increase from 281 to 595/100,000 from 2004 to 2012) it would still take over a century to reach the goal set forth by the Lancet CGS. At the current rate of progress, in 20 years, over 70% of the world’s population will be still be below 5000 operations/100,000 people. Dr. Newton emphasized there is clearly much work to be done.
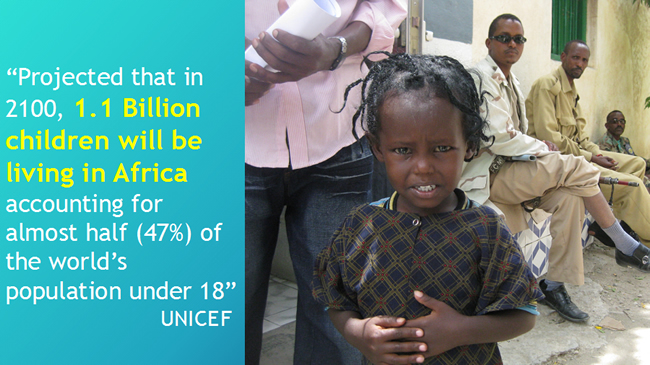
A large part of this paucity of surgical care comes from lack of safe anesthesia providers. In many countries in Sub-Saharan Africa, there are less than one anesthesiologist/100,000 people. The anesthesiologists that are trained tend to stay in the urban areas, leaving the rural areas with little to no chance of receiving safe anesthesia care. In addition to this lack of anesthesia providers, Dr. Newton highlighted the UNICEF projection that by 2100, 1.1 billion children will be living in Africa, accounting for almost half (47%) of the world’s population under 18, while stressing that this projection is the most important point in the discussion.
Dr. Newton then focused his presentation on designing a long-term model for capacity building for pediatric anesthesia and surgery in the low-resource setting. This model includes physician educators from around the world committed to move to low/middle income countries for set periods of time. This will allow them to learn the culture, perform a needs assessment, and learn to utilize local resources in order to better educate the local learners so that they can then become the educators. In Kijabe, Kenya, where Dr. Newton works, they have focused on a parallel pediatric surgery and pediatric anesthesia hybrid-training model. This model consists of a foundation of educators who have moved to and remained in Kijabe for two to 10 years as well as strategic short-term educators, who come for two to four weeks at a time. This allows for a blended faculty consisting of both African and non-African physicians with the expectation that those trained under the model will return to their home countries to lead and train more African surgeons and anesthesia providers. The longer-term physician educators travel to surrounding countries for shorter stints to provide clinical care and education while partnering with African leaders in their institutions within their education plans.
The pediatric surgery fellows are trained and mentored by surgeons who live in Kijabe and also educated by visiting surgeons. All educators use an education curriculum with deliverables that are specific to the African region. The surgical trainees are required to do a month of anesthesia training in order to understand the anesthesiologist’s role and improve their ability to assist in situations when it’s appropriate. After the year 2020, the pediatric surgery fellowship will have 10 graduates who will be operating in more than eight countries in Africa. Today, 75%, are involved in some form of education, primarily residents in general surgery, and soon three will actively be involved in pediatric surgery education.
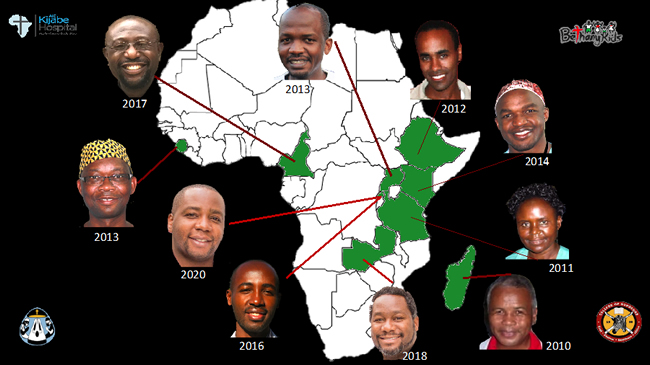
Pediatric Surgeons trained in Kijabe
Dr. Newton highlighted the Pediatric Anesthesia fellowship out of the University of Nairobi, the first anesthesia fellowship of any kind in East Africa, which was started in 2013 and is sponsored by the SPA and WFSA. The fellows rotate through Kijabe for two intense months of their pediatric anesthesia training. These fellows are carefully selected from all over Africa with the understanding they will return home to propagate and facilitate the development of pediatric anesthesia training programs. Through collaborative education efforts across many institutions from all over the world, including the development of a monthly video case conference called Safe Pediatric Anesthesia Network or SPAN, the education of these fellows has been exhaustive. Since its inception, the fellowship has graduated 14 anesthesiologists in pediatric anesthesia from seven African countries. The next steps will involve starting pediatric anesthesia fellowships in the graduates’ respective countries under their leadership.

Pediatric Anesthesia Fellowship Graduates
Dr. Newton then discussed the efforts to evaluate the education provided to the pediatric anesthesia fellows training in East Africa following graduation by hosting a Managing Emergencies in Pediatric Anesthesia (MEPA) course that utilizes the new Center for Medical Simulation and Patient Safety in Kijabe to reinforce all the skills acquired during their training so they can continue to safely train more providers.
Dr. Newton closed his presentation with the personal testimonies of several of the pediatric anesthesia fellow graduates, as well as the comparison of philosophies utilized by Kenyan marathon runners for building pediatric surgery and anesthesia capacity models:
- Be mentally prepared: it takes years to see results
- Start off slow, ease into it
- When it hurts, keep going, do not expect it to be easy
- The hardest paths will prepare you to finish the race
- No imported energy bars, just use what is local-ugali! i.e. use local resources!
- Never do it alone-partner with those who know the road
Overall, his presentation was an extraordinary example of how we can utilize our knowledge and skillset to educate healthcare providers in low income countries so they can then utilize this training and knowledge to continue, or begin providing safe surgery for children in their countries. This model is an example of anesthesiologists and surgeons working together as a team to train safe surgery/anesthesia providers for an entire country in Africa. In conclusion, he challenged the SPA, each of us, to become more involved in caring for the world’s children within a collaborative effort based upon education and education of educators, focusing on the low and middle-income countries where the imbalance is dramatic. We can make a difference!