Annual Meeting Reviews
Session V: Infectious Disease
By Constance Monitto, MD
Johns Hopkins University
The fifth session focused on infectious disease and was moderated by Mary Ellen McCann MD, MPH (Boston Children’s Hospital). Bridget Pearce MD (CS Mott Children’s Hospital) opened the session with a talk titled “SSI: Strategies for Control in Your Practice.” Her learning objectives included a review of surgical site infection metrics, a summary of national accountability, delineation of a team approach, and reinforcement of individual responsibility. Dr. Pearce reported that SSI’s exact a high cost in both dollars and lives. They are the most common healthcare-associated infection, and up to 60% are preventable. While the ancient Greeks viewed disease as a divine punishment, in the mid 1800’s Ignaz Semmelweis noted that postpartum endometritis infection rates were much higher with medical student and physician deliveries than those performed by midwives. Attributing this difference to physicians going directly from the morgue to the delivery room, he introduced hand-washing rules which greatly reduced postpartum mortality rates despite significant resistance to his ideas at the time.
Fast forwarding to 1999, the Institute of Medicine published “To Err is Human.” This sentinel report on hospital-associated adverse events was followed by an executive order by the Clinton administration to implement techniques to reduce medical errors, Congressional hearings on patient safety, and appropriation of $50 million to the Agency for Healthcare Research and Quality to reduce medical errors and help protect patients from medical mistakes. More recently the Joint Commission has delineated National Patient Safety Goals, effective January 1, 2015, which include an objective to reduce the risk of health care-associated infections. Strategies to achieve this goal include compliance with hand hygiene guidelines, implementation of evidence-based practices to prevent surgical site infections, and using proven guidelines to prevent catheter-related line infections.
The incidence of surgical site infections in children is 1.8%, but it is 3% in neonates. While some risk factors in children, such as younger age, are uncontrollable, others, such as delivery of appropriately timed antimicrobial prophylaxis and maintenance of normothermia, can be controlled. Failures to maintain best practices with regard to these controllable variables are at times due to oversights and poor communication. As a result there is now a focus on adopting a team approach including the use of safety checklists, a technique that has seen great success in decreasing risk in the airline industry. Importantly, surgical safety checklists have been shown to reduce medical complications as well, including surgical site infection rates. Finally, Dr. Pearce reinforced the importance of individual responsibility in areas such as hand hygiene as yet another way to decrease the risk of surgical site infections in our patients.
Justin Lockman, MD (Children’s Hospital of Philadelphia) continued the session with a talk focusing on “Operating Room Infections.” His objectives were to discuss common and unusual infections in the operating room focusing on which infections we should worry about spreading or catching, and which should push us to postpone surgery. Focusing on spreading infections he reported that there are two major risks for our patients – direct contact with our patients and parenteral transmission. He reported that while most centers use contact precautions to try to stop the spread of infections like MRSA, there is no data to support their efficacy, and they can be associated with decreased satisfaction with care. He informed the audience that 45% of wounds are contaminated at closure, and airborne contaminants including shed skin cells and suspended floor dust may play a contributory role in the development of wound infections. Considering intravenous transmission, viral transmission is related to failure to adhere to infection control principles, but bacterial contamination is more widespread and problematic. When studied, 15% of syringe contents were found to be contaminated and anesthesia machine switches can also be contaminated, with a co-infection rate of 13% between ventilators and syringes.
There are also diseases that we as providers may be at risk for catching or bringing home, including measles, tuberculosis, MRSA, and HSV. Protection for anesthesiologists includes vaccination and respiratory precautions such as N95 masks and PAPRs for airborne diseases. Finally, we all encounter patients in our practice with infections and must make decisions as to when to delay surgery. In some situations where the patient is profoundly ill but requires surgery to treat the source of the illness (e.g., sepsis), we should proceed but include goal-directed therapy in our management. More frequently, however, we see children come to us with minor illnesses, such as URI’s. Because URIs are so common in children it is impractical to cancel all surgeries and instead we may need to use decision trees that take into account patient, anesthetic and surgical factors in order to determine when it is best to cancel a case or proceed.
Lizabeth Martin, MD (Seattle Children’s Hospital) presented the final talk of the session, “Infection Prevention in Anesthesia Practice.” Her talk focused on quality improvement processes and practice changes initiated at Seattle Children’s in order to decrease their incidence of bloodstream infections. As discussed earlier, Dr. Martin reiterated that bloodstream infections increase patient morbidity, mortality, and health care costs. Because they are considered “preventable harm” there are also financial consequences resulting from pay-for-performance policies. Citing the 2006 New England Journal of Medicine article “An Intervention to Decrease Catheter-Related Bloodstream Infections in the ICU” by Pronovost and colleagues, she discussed the implementation of PICU best practice bundles to decrease the incidence of catheter-associated blood stream infections.
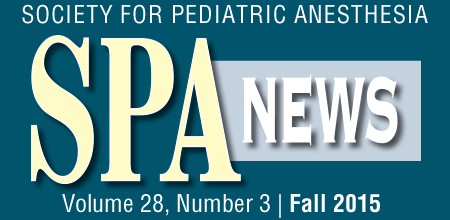
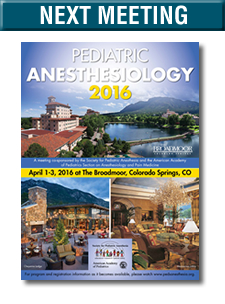
While these interventions were successful at her institution in decreasing these infections, they found that PICU patients who went to the operating room remained at increased risk. In studying this problem they identified potential contributing factors such as anesthesiologists’ incomplete knowledge of and compliance with hand hygiene as well as the challenge of having to concurrently manage a “dirty” airway and “clean” intravenous medications. They subsequently formed a multidisciplinary team to study their practice patterns and identify areas for improvement. This approach resulted in a number of changes in practice, including making hand sanitizer more available, providing a uniform IV start set, uniformly cleaning rooms, and developing a uniform “clean technique” that was developed by training and coaching physicians in the operating room (see images 1 and 2). Using these techniques they were able to further decrease the incidence of hospital-acquired catheter-associated bloodstream infections.
Image 1: Anesthesia work space divided into “dirty” gloved area (anesthesia machine and airway supplies) and “clean” ungloved area (medication manifold, anesthesia cart and computer with swinging arm)
Image 2: Medication manifold provides ability to give multiple drugs during a case without line contamination