spa-aap reviews
Friday Session IV - Achieving Excellence One Step at a Time
Reviewed by Jennifer K. Hansen, MD
University of Kansas Hospital
Improving patient safety and using technology to prevent medication errors
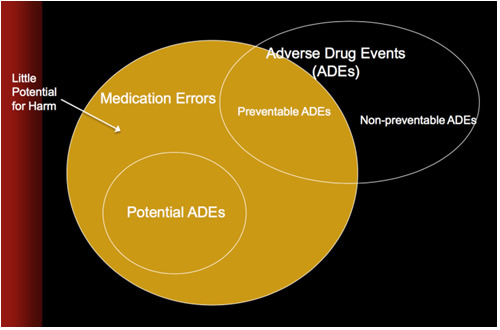
Karen C. Nanji, MD, MPH, (Massachusetts General Hospital) began this session by addressing the topic of medication errors and adverse drug events. She explained that a medication error is the use of an incorrect medication plan or action to achieve a patient care aim, or failure to complete a required action in the medication use process. Medication use includes prescribing, ordering, dispensing, preparing, administering, and monitoring after a medication has been given. An example of monitoring after medication administration would be checking the glucose level after insulin has been given. Medication errors can occur with or without patient harm.
Next, Dr. Nanji defined an Adverse Drug Event, which is patient harm or injury due to a medical intervention related to a drug, regardless of whether an error in the medication process occurs. She illustrated how a percentage of Adverse Drug Events can be avoided by preventing medication errors.
Medication errors occur in hospital wards, outpatient clinics, critical care units, and during simulation exercises, despite computerized medication dispensing, computerized physician order entry, electronic prescribing systems, electronic decision support, alerts, barcode-assisted administration, and multiple-provider checks.
The perioperative setting is particularly error-prone due to the unique medication use process which bypasses standard safety checks in a high stress, high stakes, fast-paced environment. The historical literature on medication error is sparse, largely self-reported, and prone to inaccuracies.
Cognizant of the bias associated with self-reported data, Dr. Nanji used observational study methodology to detect and report medication errors and adverse drug events at a tertiary care center1. Fully trained anesthesiologists and nurse anesthetists directly observed randomly selected operations and flagged potential errors. An adjudication committee composed of clinical and medication error experts reviewed the observer data and chart review data.
Two hundred seventy seven operations were observed. Of the 3,671 medication administrations, there were 193 medication errors or adverse drug events, which was 5.3% of all administrations. Types of errors included labeling errors, wrong dose, wrong drug, wrong timing, omitted medication or failure to act, documentation errors, monitoring errors, and inadvertent bolus. They found no correlation with patient age, sex, ASA score, BMI, procedure type, or provider type.
They found that procedures lasting longer than six hours had higher rates of medication error and adverse drug events (p<0.0001) and that administration of more than thirteen medications led to higher medication error event rates (p=0.02) and adverse drug event rates (p=0.002).
Dr. Nanji proposed solutions that use technology and process changes to reduce medication error. These solutions include:
- Bar code assisted anesthesia documentation.
- Decision support and alerts. For example, scanning a medication prior to administering it allows decision support and alerts to be activated.
- Process changes that reduce the opportunity for workarounds; make the easiest course of action the safest one. A simple process change is connecting infusions to the IV port closest to the patient to prevent inadvertent boluses.
In summary, in this study, one in twenty medications given resulted in a medication error or adverse drug event. The next steps for improvement are to design and prioritize decision support rules for the perioperative setting, develop and implement a clinical decision support tool for use in the OR, and evaluate whether the decision support tool reduces the incidence of medication errors.
Can you design your workspace to reduce errors?
Eliot B. Grigg, MD (Seattle Children’s Hospital) started with an overview of his objectives:
- A review of design principles and how design principles have or have not been applied to health care,
- understand how design can be used to improve patient safety, and
- apply design principles to improve safety at other institutions.
Dr. Grigg began by reminding the audience that most airplane crashes are the result of human factors or limitations, despite the perception that the airline industry is composed of people with the “Right Stuff”. In the automobile world, traffic signs, traffic lights, and driving lanes are designed around human limitations. Similarly, he proposed that anesthesia morbidity is due to human limitations in medication delivery.
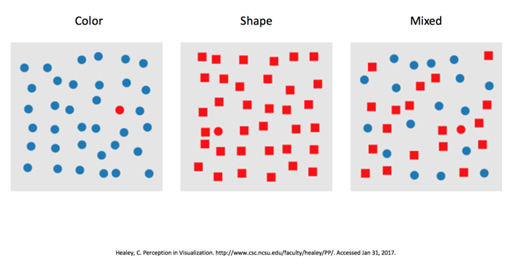
Complex decision cycles are an interaction of observations, orientation, decision making and action. There are degrees of difficulty involved in a simple task such as recognizing a red dot on a piece of paper. One can quickly and easily find a single red dot in a field of blue dots. It is harder to find the red dot quickly in a field of red squares, and even more difficult to find the red dot in a field of mixed blue dots and red squares.
Observation of a standard anesthesia setup reveals that the left, or Medication side has few safety tools, compared to the right, or Machine side which has many safety features. For example, the Medication side lacks dose checking, has no alarms, and no way to detect errors. Whereas the Machine side has color-coded gas lines, the diameter and pin-index safety systems, the oxygen-nitrous coupler, pressure and flow sensors and alarms, keyed and colored vaporizer fillers, patient monitors, and many more safety features.
A Failure Mode and Effects Analysis identified five steps in the delivery of anesthesia medications; prescribe, prepare, dispense, administer, and record and monitor. The analysis further revealed sixty-eight possible failure modes in the medication cycle of delivering one medication. Medication delivery relies on accuracy and vigilance in a high risk environment.
There are different levels of ‘mistake proofing’.
- Eliminate the error (an example on the machine side is the pin-index system),
- detect the error,
- detect the defect, and
- use cognitive aids or checklists.
In design theory, good design is invisible, is inherently intuitive, and accounts for human factors and limitations. Good design enhances performance. Bad design results in experiences that are odd, frustrating or dangerous.
Seattle Children’s Hospital tackled the problem of medication error with design theory. They first looked at medication trays. The old trays had many options, with twenty-two medications in vials arranged alphabetically. High and low use, as well as high and low risk medications were put together, and many vials looked similar, making it easy to inadvertently swap vials of medications.
The new medication tray design divides drugs into two trays; a Primary tray containing seven medications that are used 85% of the time, and a Secondary tray containing nine medications that are used 15% of the time. Design themes of 1) simplification, 2) separation between and within classes of drugs, 3) orientation, 4) signifiers and grouping (for example, the entire muscle relaxant bin is red), and 5) par levels have resulted in efficiency and cost savings.
The second design change they incorporated was the use of pre-filled syringes. Pre-filled syringes eliminate the preparation step of medication delivery, which accounts for six sub-steps and nineteen of the sixty-eight potential failure modes. Using pre-filled syringes is an example of Level 1 mistake proofing, similar to fail-safe designs in the anesthesia machine.
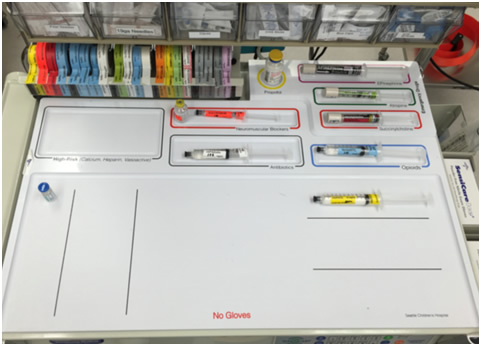
The third design change was the creation of an anesthesia medication template that organizes medication syringes and the workspace by creating a space for each medication. The workspace is organized using multiple signifiers such as location, color, labeling, and white space. This standardized the workspace while still allowing flexibility and acceptance of the template.
To study the impact of these design interventions, Dr. Grigg and associates at Seattle Children’s used simulation to compare performance in emergency scenarios with and without the medication template2. They simulated emergency scenarios using 41 participants in 82 scenarios performing a total of 328 medication administrations. They found that the odds ratio for medication errors using the Anesthesia Medication Template was 0.21 (p<0.01) and that most errors were due to calculation and delivery errors, not syringe swaps.
They tracked the mean monthly error rate per 1000 anesthetics for twelve months before and after implementation of the medication template. Overall medication errors were significantly reduced from 1.5 to 0.83 per 1000 anesthetics; medication swaps, preparation errors, miscalculations and timing errors were also significantly reduced from 0.8 to 0.26 per 1000 anesthetics. The incidence of errors causing harm, 0.22, was unchanged.
Finally, Dr. Grigg summarized his talk by saying that we are still in the “Right Stuff” era for medications and that we are lacking a singular vision for the ‘left side’. Design is a way of seeing, simplifying, and asking the right questions. He ended with a challenge: “Let’s make it hard to do wrong and easy to do right.”
Improving practice through QI: pursuing perfection, attaining excellence
Anna M. Varughese, MD, MPH (Cincinnati Children’s Hospital) began her talk by asking the question “Why are there no Toyotas in healthcare?” referring to two events:
- the publication of two books that described the Lean method in the auto industry and business, and
- the Institute of Medicine report “Crossing the Quality Chasm”, that called for a fundamental redesign of the US healthcare system to achieve improvement in safety, effectiveness, patient centeredness, timeliness, efficiency, and equity.
Quality improvement approaches and tools come from IHI-QI, the Institute for Healthcare Improvement Quality Improvement, Lean Six Sigma and Evidence Based Medicine models. The guiding principles for implementation of a successful QI initiative include:
- simple initiatives – having one key goal and one key change increases success,
- interdisciplinary teams,
- early adopters that help spread new ideas,
- rapid pilots that make implementation of change manageable,
- providing rapid feedback to the teams affected by the initiatives, and
- advertising the gains from the initiative.
The drivers for transformational change and sustained improvement are leadership commitment, standardization and accountability, alignment, integration, assimilation, and transparency.
An example from Cincinnati Children’s Hospital was the work of the Cincinnati Children’s Hospital Medical Center (CCHMC) Spine Efficiency team, which included representatives from orthopedics, perioperative nursing, anesthesia, data management and quality improvement. Their goal was to improve efficiency, flow, and access to the operating room without adding resources. Specifically, they sought to improve on-time completion of posterior spinal fusion surgery for adolescent idiopathic scoliosis patients. The team developed expectations for the process of patient readiness, for example, ‘in the room’ by 7:30 am. Part of the process included standardization of the patient preoperative timeline. An information handout was given to families. A follow-up survey showed that the handout was well received, increased families’ understanding of the perioperative process and gave them better planning ability.
The team created a case summary for each surgical case, based on five case events; time to in-room, anesthesia start time to anesthesia ready, anesthesia ready to incision, incision to close, and close to wake up. After implementation of the efficiency measures, variance in the actual time for posterior spinal fusion surgeries compared to prior surgeries of the same type was reduced.
Using Lean methods, the Neurosurgery Efficiency Team, another CCHMC multidisciplinary team, came up with interventions for reducing neurosurgery cases from 152 minutes to 100 minutes. They were able to increase the number of cases completed in a 10-hour block from three to five, increase the percentage of first start cases actually starting on time from 60% to 80%, and had a 50% reduction in the percentage of patients delayed for more than two hours. Families were given updates on their expected surgery time, with a standardized script around delays, and families were offered meal tickets for two hour delays. Neurosurgery developed an app for patients’ families that allowed them to access information about providers and have other questions answered. As a result of these quality improvement measures, patient satisfaction was improved and neurosurgery achieved the highest ranking for surgical patient satisfaction at CCHMC for the second half of 2016.
Dr. Varughese ended her talk by quoting Vince Lombardi, “Gentlemen, we will chase perfection and we will chase it relentlessly, knowing all the while we can never attain it. But along the way, we shall catch excellence.”
Panel Question and Answer, moderated by R. Blain Easley, MD
Question:
Inquiry about the Color Coded Medication Template developed and used at Seattle Children’s Hospital; is it available for everyone? And could it be used between institutions?
Answer:
(Dr. Grigg) The template is not proprietary. Currently, Seattle Children’s has two different templates, one for cardiac/transplants, and another one for everyone else.Question:
Regarding the analogy of Toyota, how do we give excellent care to patients who are different, and not like the parts of a car?
Answer:
(Dr. Varughese) QI helps us to better deliver care by simplification and standardization. We customize our care to the patient and standardize the delivery.Question:
Another question regarding Cincinnati Children’s and the Neurosurgery Efficiency team: How did Cincinnati Children’s get ‘buy-in’ from nursing to go from three to five cases per day?
Answer:
(Dr. Varughese) Efficiency decreases frustration on the patient side, but also on the provider side, including physicians and nurses.
References
- Nanji KC, Patel A, Shaikh S, Seger DL, Bates DW. Evaluation of perioperative medication errors and adverse drug events. Anesthesiology 2016; 124:25-34
- Grigg, E, et al. Assessing the impact of the anesthesia medication template on medication errors during anesthesia: a prospective study. Anesth Analg. Accepted Nov 17, 2016.