SPA-AAP Reviews
Friday Session II – Enhanced Recovery After Surgery
 Reviewed by Chris D. Glover, MD, MBA
Reviewed by Chris D. Glover, MD, MBA
Texas Children’s Hospital
Session II centered on a highly anticipated current topic in perioperative medicine: enhanced recovery after surgery (ERAS). Ty Muhly, MD (Children’s Hospital of Philadelphia), Megan Brockel, MD (Children’s Hospital of Colorado, Denver), and Sanjay Krishnaswami, MD (Oregon Health & Science University, Portland) all reported on their respective efforts toward incorporating enhanced recovery pathways and some of the common aims and pitfalls associated with their implementation effort.
Historically, most consider Henry Kehlet, MD, PhD to be the pioneer for the concept of ERAS given his work on outcomes following colorectal surgery. Dr. Kehlet defined the key components for ERAS pathways as:
- A multidisciplinary team.
- A multimodal approach to reducing complications.
- The use of evidence based protocols.
- Continuous process improvement.
All of the speakers noted the relative dearth of available ERAS data in the pediatric population. Dr. Krishnaswami reported that a previous meta-analysis included only five pediatric studies over the last decade that incorporated portions of the 20 parameters defined as part of an ERAS pathway.
For background, Dr. Muhly reported on the adult literature in ERAS. Evidence on the effectiveness of enhanced recovery was specifically cited via a 2014 meta-analysis that covered sixteen randomized controlled trials involving 2400 patients. Consistent findings from this meta-analysis included reduced non-surgical complications, reduced length of stay, and no change in rates of readmission.
Care paradigms associated with ERAS are usually broken down along phases of care as listed in this figure for bowel surgery.
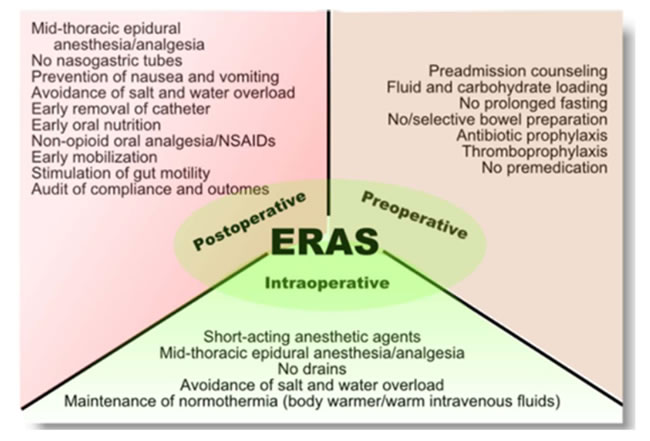
Fig 1. ERAS pathway for colorectal surgery
What is particularly interesting from this figure is how the formulation of these multidisciplinary teams forced a critical assessment of dogma. Long held treatments considered appropriate for care such as bowel prep, extended NPO times, and placement of nasogastric tubes have largely been removed from care pathways to improve the time to return of normal bowel function. While enhanced recovery could be considered a criticism of our specialty given our place in perioperative medicine, Dr. Muhly rightly points out that enhanced recovery has prioritized extended communication across teams and across phases of care.
Dr. Muhly then covered his experience incorporating an ERAS pathway at his institution. Combining components from six sigma, lean and advance quality improvement has yielded the CHOP improvement framework (Fig 2), which includes defining a problem, diagnosing the problem via measurement and analysis, testing and implementation of solutions, and sustaining results.
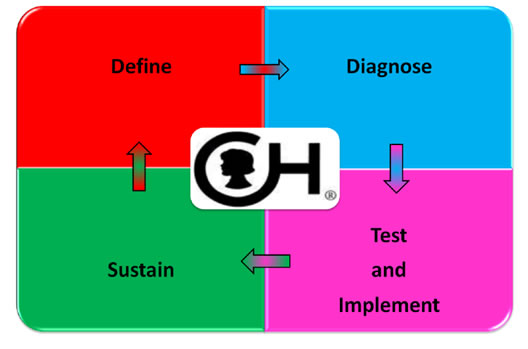
Fig 2. CHOP Improvement Framework
Dr. Muhly used this framework for idiopathic scoliosis with the primary aim of formalizing a recovery pathway. The primary outcome measure was length of time to functional recovery and by proxy the length of stay. Diagnosis of this required fostering a multidisciplinary team, taking a critical assessment on the recovery process, and creating protocols all combined with developing data tools to assist with sustaining the process flow improvement. What seemed especially important was ensuring that the protocols were explicit, granular, easily accessible, and available. Testing and implementation required extensive communication and buy-in across specialties (pain, surgery, anesthesia, physical therapy). Sustaining the results centered on communication and a critical assessment to further improve workflows.
Incorporation of idiopathic scoliosis into this framework yielded some impressive results. CHOP has noted a decrease in median stay from about 5 to 3.5 days and improvements in pain scores through all phases of care. Following this success, Dr. Muhly also set about decreasing care variance for the pectus excavatum population. Trends thus far have been positive with length of stay dropping from a median of 5 days to 3.5 days. Secondary metrics such as PCA discontinuation and population discharge statistics also point toward advocation of ERAS implementation.
Dr. Brockel’s discussion had a similar feel. She focused on her center’s experience on implementation of an ERAS pathway for urologic reconstruction cases.
Dr. Brockel pointed to global goals of ERAS as:
- Maximizing pain control.
- Minimizing metabolic stress.
- Optimizing fluid balance.
Outcomes metrics noted include significant reductions in return of bowel function, shorter hospitalizations, and lower overall complication rates by roughly 50% in the recovery phase.
Dr. Brockel also emphasized breaking down phases of care to create and develop an ERAS pathway as one would for any patient undergoing surgery with a critical evaluation of previously held dogma. Preoperative examples mirrored Dr. Muhly with advocation of avoiding bowel preparation, minimizing fasting times, and avoidance of NGT tubes. The use of multimodal analgesic regimens to minimize opioid use as well as judicious fluid management were reported by Dr. Brockel as contributing to early mobilization and recovery. Her institutional efforts for ERAS implementation in urologic reconstruction also yielded positive results. A consistent theme communicated by the speakers relates to the ubiquity of ERAS protocols. The protocol at Children’s Hospital of Philadelphia has been embedded into the EPIC electronic medical record while the protocol at Children’s Colorado is available for any practitioner via the institution’s SharePoint site.
The intraoperative protocol consisted of both wound soakers placed by surgeons and single shot transversus abdominis plane blocks performed by the anesthesiologists. This was combined with dexmedetomidine infusions and scheduled acetaminophen and ketorolac in an effort to mitigate usage of opioids. When compared to historical controls, Dr. Brockel found that patients in the ERAS pathway started eating earlier with an earlier return of bowel function. Median length of stay dropped from 8 days to 5.7 days. While not significant, this seems compelling and the lack of significance seems primarily related to the sample size of the respective populations.
Given the variable adherence and compliance at her institution, Dr. Brockel noted an interesting phenomenon upon review of available data. If compliance was <50%, roughly 70% of patients experienced symptoms that delayed discharge. Further, the complication rate approached 40% in this group with an average LOS of nine days. When compliance to the protocol hovered above 90%, the rate of symptoms delaying discharged dropped to 40%. The complication rate dropped by half to 20% while the average LOS dropped to six days.
Dr. Brockel reported on two major predictors for improving postoperative outcomes for those who might feel overwhelmed at incorporating ERAS pathways across institutions: receiving preoperative carbohydrate drink and perioperative intravenous fluid management. While creating a protocol seems easy, Dr. Brockel divulged that a major hurdle at her institution was in convincing colleagues of the value of using of protocols to standardize care. She further reported that by demanding strong local leadership via local champions, combined with the formation of multidisciplinary teams with dissemination of results to continually engage stakeholders, might allow for improved success in implementation of ERAS pathways at respective institutions.
The last speaker provided a view of enhanced recovery from the surgical perspective. Dr. Krishnaswami from the Oregon Health and Science University (OHSU) actually discussed the incorporation of ERAS pathways into fellow education to facilitate reaching milestones for competency-based education (Fig 3).
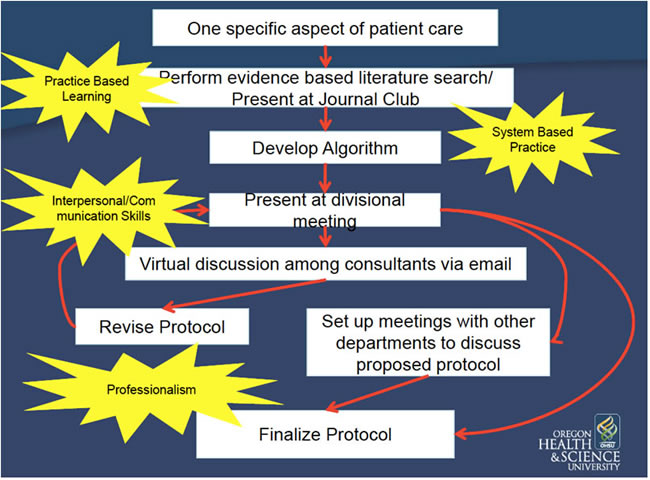
Fig 3. Oregon Health and Science University – ERAS and House Staff Milestones Pathway
Dr. Krishnaswami specifically pointed to the dearth of available data for pediatric patients on enhanced recovery. From his perspective, an ERAS program centered on minimizing variance in care allows for continuous quality improvement. Using a guiding principle of minimizing variance to provide better value-based care as a good thing evolves this process into a care standardization program for all involved. Use of pediatric surgery fellows in initiating and incorporating these pathways through the system allows for assessing multiple elements of competency-based education. On its face, it would seem successful incorporation of any process/pathway by the fellows requires competence in communication, professionalism, problem-based learning, system-based practices, and patient care.
While this process was confined to one service line (pediatric surgery), the data remains compelling. Dr. Krishnaswami reviewed a couple of their ERAS pathways. The gastrostomy protocol at OHSU pointed to decreases in LOS and decreases in overall cost. Secondary metrics such as postoperative ER visits and phone calls to providers were also decreased. Another reported protocol covered non-perforated appendicitis. When compared to controls, statistically significant findings include decreases in length of stay. The complication rate did not change, but there was a small associated increase in the cost to deliver this care. Surgeon compliance to the protocol was 93%, which points to acceptance of this standardized care pathway if patients present with this issue. Comparing all enhanced recovery efforts at OHSU yielded some impressive findings. Approximately 400 patients have been guided through one of several ERAS pathways. When compared to controls, LOS was down by one day. Complication rates decreased from 21% in control to 11% in the ERAS pathway. Milestone scores were also higher for fellows with incorporation of patients in these care pathways. While it is important to point out the lack of other service line involvement, future plans by the surgical services at OHSU point to expanding care protocols across service lines.
The overarching message for incorporation of ERAS pathways at institutions is that it remains complex. Data no doubt shows improvement in patient outcomes when ERAS pathways are used as evidenced by decreased variance in care, decreased length of stay, and decreased complication rates. The lack of available pediatric data should not serve as a deterrent to efforts at standardizing care. Local leadership amongst service lines, combined with readily accessible protocols, along with communication amongst shareholders should facilitate widespread acceptance of enhanced recovery for pediatric patients undergoing surgery.